F. Mitu1,2, Daniela Boişteanu1,3, Adina M. Ţurcanu1,3
Article received on the 18th of October 2012. Article accepted on the 7th of February 2013.
1 “Gr. T. Popa” University of Medicine and Pharmacy, Iaşi, Faculty of General Medicine, Department of Medical Semiology
2 The Hospital of Clinical Rehabilitation of Iaşi, Clinic for Cardiovascular Recovery
3 Clinical Hospital of Pulmonary Diseases of Iaşi
E-mail: adinagheorghita@yahoo.com
Abstract: The severe forms of sleep apnoea often lead to sudden deaths, and the implementation of an efficient treatment leads to the normalisation of patients’ lives by using this pathology. We report the case of a patient, aged 60 years, with morbid obesity and essential hypertension, who came for cardiovascular re-evaluation, and accused sleepiness, dyspnoea degree III mMRC, excessive diurnal sleepiness, memory and focus problems. Up to the admission, the patient has not benefitted from an expert opinion for a correct diagnosis. Following the clinical and paraclinical investigations, it is given the diagnosis of highly severe sleep apnoea, which requires permanent ventilation with positive pressure throughout the sleep periods.
Keywords: apnoea, hypertension, obesity
INTRODUCTION
Sleep apnoea is among the most frequent chronic disorders. Obstructive sleep apnoea is defined as an interruption of the airflow with persistent effort to breathe, while central apnoea represents an interruption of the airflow with absence of the effort to breathe. Hypopnoea is defined as a reduction of at least 30% of the flow, associated with a minimum reduction of 4% of the Oxygen saturation. The apnoea-hypopnoea index (AHI) represents the total number of apnoeas and hypopnoea occurred throughout the entire sleep period. The SAHS severity is classified according to the number of episodes per hour: slightly – 5-10 episodes/hour, moderate – 15-30 episodes/hour, severe – more than 30 episodes/hour1,2.
The risk factors of obstructive sleep apnoea are age, obesity, male gender, familial and genetic predisposition, smoking and alcohol, medical co-morbidities (high blood pressure, congestive heart failure)3.
In cardiology, sleep apnoea might influence the incidence and control of the systemic blood pressure. The action mechanism is not precisely known, but the presence of hypoxia associated to apnoea may determine an increased sympathetic activity and, therefore, the occurrence of high blood pressure. Some researchers proved that sleep apnoea occurs in 30-50% of male patients suffering from high blood pressure, and more than 90% of the patients with apnoea included in the study already had high blood pressure4,5.
In addition, sleep apnoea registers an increased importance among patients with type II diabetes.
Case presentation
We present the case of a patient, aged 60 years, who came to the Clinic for Cardiovascular Recovery of Iasi for dyspnoea degree III mMRC, vertigo, fatigue, excessive diurnal sleepiness, diurnal asthenia, focus difficulties, memory problems and tinnitus.
From the hereditary and collateral history, it is observed a familial aggregation of the cardiovascular pathology and of type II diabetes.
Six years earlier, the non-smoker patient had received the diagnosis of essential hypertension (maximum value of the systolic blood pressure of 170 mmHg), type II diabetes, treated with oral antidiabetic drugs.
Clinical examination on devices and systems reveals a body weight of 136 kilos and a body mass index of 54 kg/m2, bilateral leg oedema, bilateral knee pain at joint mobilisation.
Considering the admission reasons and the clinical examination, it was suspected that the patient suffered from sleep apnoea syndrome, and additional investigations were recommended.
Thoracic imaging indicated an emphasized pulmonary drawing of bilateral interstitial type, ecstatic thoracic aorta, left inferior arch of the heart sticking out. The performed spirometry was normal.
The ENT examination identified the papillomatosis of the palate veil, without any obstructive effect, chronic hypertrophic rhinitis and also aroused the suspicion of sleep apnoea.
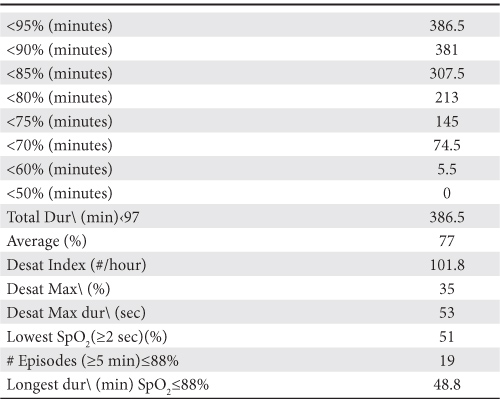
Due to the suspicion of this diagnosis, it was recommended to perform a respiratory polygraphy within the sleep laboratory of the Hospital of Pulmonary Diseases. The result of the polygraphic records indicates the presence of sleep apnoea of obstructive type, very severe, with an AHI index = 101/sleep hour, a desaturation index of 101/hour, Oxygen nocturnal average saturation 77% (Tables 1 and 2). It was commenced ventilation with positive pressure via nasal mask. Self-titration of the positive pressure via the nasal mask led to a pressure of 12.2 mBarr and to the occurrence of only three remaining apnoeas. Therefore, it was advised to use an APAP device adjusted between 4 and 16 mBarr, with humidifier, at least five hours a night, for an unlimited period. In addition, the patient will come for follow-up after 1, 3, 6, 12 months, and then annually.
Table 1. Type of events recorded through poligrafy
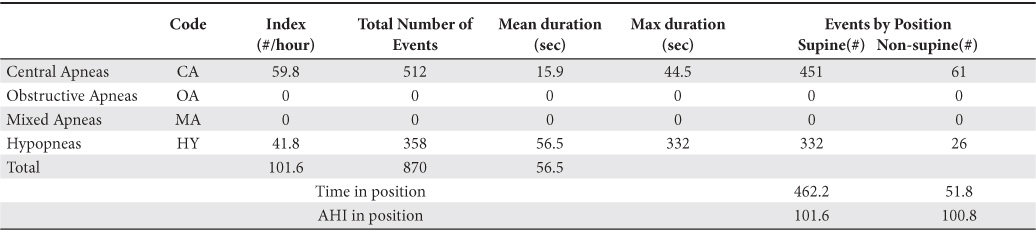
Table 2. Oximetry distribution
The analyses performed in order to highlight sleep apnoea complications and associated pathology lad to the treatment’s subsequent implementation.
The echocardiography highlighted calcifications of the anterior aortic ring, atheromatosis of the posterior aortic ring, mitral deficiency degree I Doppler. Carotid ultrasound highlighted calcified plaques at the bifurcation of the right carotid, small calcified plaques on the left carotid bifurcation. The ankle-right arm index was 1,13, and left arm 1,36. The 24-hour monitoring of the blood pressure revealed high values of the blood pressure, the highest being 171/89 mmHg and the lowest 128/64 mmHg.
The eye exam identified lens transparency disorders, retinal angiosclerosis stage III, peripheral pigmentation disturbances.
Haematological and biochemical blood tests revealed the presence of an inflammatory syndrome (VSH= 82 mm/hour, fibrinogen= 7.90 mg/dl, CRP= 3.77) and of hyperuricaemia (uric acid 8, 64).
The advised basic system was ventilation with positive pressure via nasal mask, in accordance with the established indications, continuation of the treatment with oral antidiabetic drugs, nebivolol 10 mg per day, olmesartanum 40mg per day, allopurinol 100 mg three times a day, colchicine 1 mg per day, hyposodic, hypocaloric diet, kinetic therapy at home.
After a month with nocturnal APAP ventilation at home and compliance with the indications, the patient’s condition returned to normal. The clinical and paraclinical examination reveals an important weight loss (12 kilos), increase of the effort capacity, an overall improved condition, AHI index remaining at 3/sleep hour and the same efficient pressure to continue nocturnal ventilation.
DISCUSSIONS
Sleep apnoea is a pathology, which must not be neglected because it can lead to sudden death. In the said case, a very severe form was diagnosed (AHI-101/sleep hour with desaturation index = 101/hour and average SpO2 = 77%), which could have led to death at any time during the sleep.
The patient’s weight status (BMI = 54 kg/m2), as well as the increased diameter of the neck represents another severity factor. In this case, weight loss will lead to an improvement regarding the effort capacity and the apnoea form. Therefore, there are recommended a hypocaloric diet, respiratory rehabilitation and kinetic therapy.
The association of high blood pressure with sleep apnoea was confirmed over time by several studies. The systolic pressure increases more than the diastolic one; the variation is 1.4 ± 0.8 mmHg in relation to the Oxygen saturation change compared to the diastolic pressure (2.4 ± 1.3 mmHg), which determined the debit-volume increase by increase of the venous return during the apnoeic episodes1-3. This aspect is associated to the increase of the negative intrathoracic pressure. In this case, the patient had long apnoea episodes and high values of the blood pressure, which were controlled via drugs for a long period. At the same time, it was also observed the association of the diabetes.
A series of studies proved that SAHS influences cardiovascular risk by sympathetic activation, chronic inflammatory system, dyslipidemia and insulin resistance, oxidative stress, etc.1,2. Therefore, the treatment of a patient with sleep apnoea who also presents disorders such as essential hypertension, diabetes, morbid obesity represents a challenge for the team made up of cardiologists, pulmonologists, diabetologists, kinetic therapy physicians.
CONCLUSIONS
Sleep apnoea is associated to cardiovascular and metabolic changes and significantly contributes to patients’ mortality. It is recommended to commence treatment as soon as possible because most of the times this leads to an improvement of all parameters and of the overall condition.
Conflict of interests: none declared.
References
1. Boişteanu D, Simionescu V, Haulica I et al. Medicina Somnului, Editura Medicală, Iaşi, 2008.
2. Mihai V, Mihăescu T, Luca G et al. Apneea de somn, Editura Edit DAN, Iaşi, 2011.
3. Lawati Al, Patel SR, Ayas NT. “Epidemiology, risk factors and consequences of obstructive sleep apnea and short sleep duration”. Prog Cardiovasc Dis 2009;51:285-293.
4. Nieto FJ, Young TB, Lind KB et al. Association of sleep – disordered breathing, sleep apnea, and hypertension in a large community – based study. JAMA 2000;283:1829-1836.
5. Leung TSR, Douglas TB, Sleep apnea and cardiovascular disease. Am J Respir Crit Care Med 2001;164:2147-2165.
 This work is licensed under a
This work is licensed under a