Simina Crisan1,2, Cristina Vacarescu2, Alina-Ramona Nicola1, Mihai Andrei Lazar2, Dragos Cozma1,2, Rodica Dan1,2,
Lucian Petrescu1,2
1 Victor Babes University of Medicine and Pharmacy, Timisoara
2 Institute of Cardiovascular Diseases, Timisoara, Romania
Abstract: The management of antithrombotic treatment in elderly patients represents a great challenge in every day medical practice, taking into account both increased ischemic events risk as well as high bleeding risk as characteristics of this particular subset of patients. The great number of physiopathological changes that are found in elderly people in multiple organs and systems, mostly liver and kidneys, lead to an increase in the individual variability of therapeutic response, as well as to an augmented drug toxicity and potential decreased therapeutic benefit. Keywords: elderly patient, ischemic risk, bleeding risk, antithrombotic treatment
INTRODUCTION
Since the increase of the medium life expectancy time has been established as a modern society characteristic, the number of people over 60 years of life in the general population is constantly growing, with an estimated prevalence of over 2 billion until 20501. Regarding age, there is a general tendency of considering as “elderly” the people aged over 75 years, although, in a number of studies that have led to the elaboration of multiple risk scores, the value taken into consideration was 65 years of age2. On the other hand, the prevalence of acute coronary syndromes in this particular category of patients is a significant one, and, according to recent statistics, more than one third of acute myocardial infarction diagnosed patients and approximately two thirds of the
deceased following this pathology were over 75 years of age3. The great challenge concerning the management of antithrombotic treatment in elderly patients is generated by numerous factors that are common in these particular patients: multiple organ damage, increased bleeding as well as ischemic events risk, comorbidities and concomitant medical therapy and last, but not
least, low medical treatment adherence.
ELDERLY PATIENT: BETWEEN ISCHEMIC AND BLEEDING RISK
Antithrombotic treatment, including antiplatelet, anticoagulant and fibrinolitic treatment, is used in order to prevent or to ameliorate the severity of embolic events – stroke, acute myocardial infarction, systemic embolism, deep vein thrombosis or pulmonary embolism, as well as to ameliorate cardiovascular and any cause mortality, of course, with an associated increased
bleeding risk. The great challenge for the medical practitioner is to establish if, in the elderly patient, the benefit of antithrombotic treatment surpasses the bleeding risk, risk that can generate an increased mortality by itself4. The connection between advanced age and vascular pathology is illustrated by the increase of cardiovascular risk when aging. Thus, elderly people are characterized
by a number of modified haemostatic factors, such as the rise of procoagulants factors (fibrinogen, factor VII, factor VIII), the rise of fi brinolitic system factors such as plasminogen activating inhibitor in women and the rise in antithrombotic factors in women (C protein, antithrombin, tissue factor inhibitor), all of these having as consequence the formation of an antithrombotic
status5. This antithrombotic status, associated with modifi ed aged related blood rheology, with the increased plasmatic viscosity and erythrocytes rigidity, is contributing, along with endothelial dysfunction, inflammation and the imbalance between oxidative stress and antioxidant factors in the development of elderly patient atherosclerosis6. The administration of antithrombotic treatment in elderly is also complicated by a number of modifications related to multiple systems and organs. Related to the liver function, the decrease of hepatic blood flow and the modified structure and dimensions are contributing to the decrease of the activity of P450 (CYP) 1, 2C4 and 2D6 cytocromes. In a similar way, concearning the kidneys activity, blood flow and the kidneys
function are reduced. Constant renal function reduction associated with frequent intercurrent illnesses (heart failure decompensations, intercurrent respiratory infections) may lead to the decrease of creatinine clearence, with direct impact on the antithrombotic molecules that have a predominant renal filtration rate (low molecular weight heparines–LMWH, fondaparinux,
bivalirudine, dabigatran, eptifi batide and tirofiban). Moreover, it is recommended to evaluate the renal function using calculation formulas that are taking into account the age and the weight, beyond the simple serum creatinine value that might overestimate the renal function in this particular subgroup of patients8.
INDIVIDUALIZING ANTITHROMBOTIC TREATMENT IN THE SETTING OF ACUTE CORONARY SYNDROME
Aspirine
Aspirine is acting by the irreversible inhibition of ciclooxygenase-1, thus decreasing the thromboxane A2 production and the benefits of its administration in primary prevention of athero-thrombotic cardiovascular disease are well documented by numerous studies and meta-analyzes8. These extended research has demonstrated a decreased vascular event rate in elderly in compare to younger patients, following aspirine administration (1.53% vs. 0.40% per year)8. A recent japanese study, Japanese Primary Prevention Project, has demonstrated that in hypertensive, dyslipidemic or diabetic patients aged between 60-85 years randomized to aspirine 100 mg/day versus placebo, the administration of aspirine has halved the rate of myocardial infaction
or transient ischemic attack, but has also doubled the risk of extracranial major bleeding9. The benefit of aspirine administration is also found, without doubt, in secondary athero-thrombotic disease secondary prevention. It is also important to notice that the bleeding risk associated with low dose aspirine administration (75-100 mg/zi) is 2-3 fold higher in elderly in compare
to younger population, for both genders and that the risk of upper gastro-intestinal tract bleeding is considerably increased after 70 years of age10. Thus, the current guidelines are recommending
low dose aspirine administration (75-100 mg/day) in elderly patients with overt athero-thrombotic cardiovascular disease, in the absence of contraindications represented by allergies, active bleeding or intracranial hemorrage11. Thienopyridines: clopidogrel and prasugrel Thienopyridines (Clopidogrel and Prasugrel) are prodrugs with active metabolites that irreversibly inhibit
platlet activity by interfering with the P2Y12 receptor. Trials such as CURE (primary PCI in acute coronary syndromes), COMMIT and CLARITY-TIMI 28 (STEMI patients treated with aspirine and fibrinolitic therapy) have demonstrated the benefi ts of clopidogrel administration in a lowding dose of 300 mg followed by a maintenence dose of 75 mg/day12-14. To notice that
trials that have included patients treated with thrombolitic therapy did not include patients over 75 years of age, and thus, not knowing the effect of administerig lowding clopidogrel dosis, guidelines only reccomend the administration of maintenence 75 mg/day dose. The duration of dual antiplatelet therapy after acute coronary syndromes is stil a matter of great debate.
The DAPT trial, that included 40% of patients in the proximity of an acute coronary syndrome, compared a duration of 12 months of dual antiplatelet therapy versus an extended 30 months period of time and reported a smaller ischemic event rate in the extended dual antiplatelet therapy group, but with increased bleeding complications15. The TRITON-TIMI-38 trial, that included acute coronary syndrome patients treated with Primary PCI, aspirine and prasugrel or clopidogrel, demonstrated the superiority of prasugrel (60 mg lowding dose, then 10 mg/day) vs. Clopidogrel, but with an incresed rate of bleeding complications in the group of patients over 75 years of age16. For the moment, the recommendation for elderly patients with acute coronary syndromes is to be treated preferably with clopidogrel rather then prasugrel or ticagrelor, if they have a high bleeding risk11. The administration of prasugrel in patients over 75 years and under 60 kilograms should be cautioned and is contraindicated in patients with previous stroke or ischemic transient attack. In acute coronary syndromes without ST segment elevation (NSTEMI), it is not recommended
to administer prasugrel before angiography11.
Ticagrelor
Ticagrelor, reversibly inhibits platelet aggregation by binding with the P2Y12 receptor and is recommended in dual antiplatelet therapy along aspirine, in the treatment of NSTEMI acute coronary syndromes regardless of the management and in STEMI patients referred to primary PCI, with a recommended lowding dose of 180 mg followed by 2×90 mg/day. The main trial that demonstrated the superiority of ticagrelor vs. Clopidogrel is the PLATO trial, trial that included 15% of patients over 75 yers of age17. That is why, in the situations mentioned above, we
recommend the administration of ticagrelor associated with aspirine in elderly patients with acute coronary syndromes, in the absence of contraindications represented by active bleeding or intracranial bleeding and carefully administration in patients with history of asthma/COPD or sino-atrial advanced disease without pacemaker implantation11. We consider important to
mention that there are no evidences regarding ticagrelor administration in patients receiving thrombolitic therapy.
DUAL ANTIPLATELET THERAPY: HOW LONG?
As we have already mentioned, the duration of dual antiplatelet therapy after interventionally revascularized acute coronary syndrome is still a matter of great debate. It is now recommended to maintain dual antiplatelet therapy for up to one year and to exactelly establish the duration of therapy after considering the type of stent used for revascularization (bare metal vs. drug eluting stent) and the risk of bleeding, that is incresed by using prasugrel or ticagrelor in compare to clopidogrel11. One of the studies that have evaluated the extended dual antiplatelet therapy administration is the DAPT trial, trial that included patients without adverse cardio-vascular events during the fi rst year after primary PCI and that were randomized to either extended to additional 18 months of dual antiplatelet therapy with aspirine and clopidogrel or to prasugrel vs aspirine alone. The results demonstrated that extended dual antiplatelet therapy determined the decrease of intra-stent thrombosis rate and adverse cardiovascular events but with a significant increase in the bleeding complications rate18.
PARENTERAL ANTIGOAGULANTS: UNFRACTIONATED HEPARIN AND LMWH
Since it is not eliminated throught the kidneys, unfractionated heparin may be administered even in situations when creatinine clearence is under 30 ml/minute. Even so, in elderly patients frequent bioavalability changes may appear, as well as changes in the inflammatory status, cardiac output or body weight. Because a number of trials have established the superiority of LMWH in
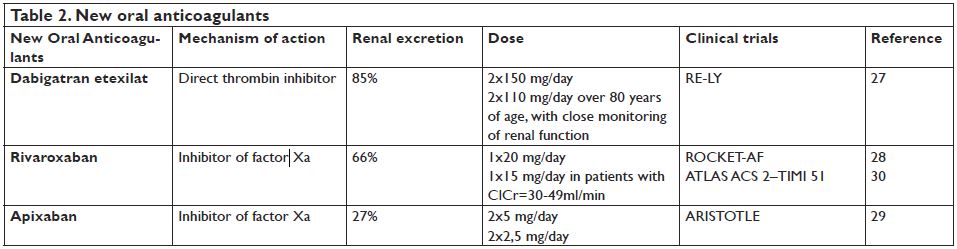
compare to unfractionated heparin concearning bioavailability and efficiency in acute coronary syndromes treated with trombolitic therapy or primary PCI, with a similar bleeding complications rate, LMWH are preferred to unfractionated heparine. One of the major disadvantages of LMWH is represented by the mainly renal elimination rate, with the need of adjusting the administered dose related to creatinine clearence (CrCl) in patients with impaired renal function. Concearning enoxaparine, it is recommended to administer 1x1mg/kg/day for values of the CrCl<30 ml/minute and abobe 75 years of age the administration of 2×0.75 mg/kg/day and no i.v. bolus for trombolitic therapy (Table 1)19.
Fondaparinux
Fondaparinux is represented by a synthetic pentasaccharide, an inhibitor of factor Xa, mainly eliminated on renal level and thus contraindicated for values of CrCl under 20 ml/minute. Since a number of studies, including OASIS-5 have demonstrated a similar ischemic events rate in NSTEMI patients treated with Fondaparinux 1×2,5 mg/day subcutaneous vs. enoxaparine
2x1mg/day for a maximum of 8 days, with a bleeding rate signifi cantlly lower after fondaparinux administration, it is recommended to administer fondaparinux in NSTEMI and STEMI patients that are not undergoing primary PCI19-21. In the case of an invasive management, bivalirudine or unfractioned heparine administration is recommended in order to prevent periprocedural
thrombotic complications (catheter thrombosis).
TRIPLE ANTITHROMBOTIC THERAPY IN ELDERLY PATIENTS – THE GREAT CHALLENGE
Since atrial fibrillation has a great risk of mortality and morbidity due to stroke and thrombo-embolic events and taking into consideration the fact that this rhythm disturbance is having a high prevalence and is representing an important health issue world wide, one of the most important indications of anticoagulant oral treatement is represented by the prevention of thromboembolic accidents in patients with non-valvular atrial fi brillation that are associating at least one risk factor for stroke22,23. That is why the current guidelines of the European Society of Cardiology for the management of atrial nonvalvular fibrillation as well as the most recent focus update on the same fi eld from 2012 recommend the use of CHA2D2S-VASc score for stratifying embolic
risk of these patients and identifying those at „low” risk, that is the ones with CHA2D2S-VASc score=0 (men) or 1 (women)22. Taking these data into consideration, the majority of patients diagnosed with atrial fibrillation (>80%) will require oral anticoagulation. On the other hand, elderly patients often present with acute coronary syndromes in the setting of another pathology that requires anticoagulation, as usual atrial fibrillation and thus, the management of antithrombotic treatement in these conditions may be a true challenge. The latest guideline of the European Society of Cardiology for the management of patients with acute coronary syndromes without ST segment elevation that are undergoing PCI is giving a straight answer to that problem21. According to that guideline, for the patients with non-valvular atrial fi brilation and NSTEMI with a low and intermediate HAS-BLED risk (0-2), triple therapy with aspirine, clopidogrel and oral anticoagulant – antivitamin K or novel oral anticoagulant, is recommended for 6 months followed by dual therapy with anticoagulant and aspirine or clopidogrel for up to one year and then oral anticoagulation for lifetime. For the patients that are having a high bleeding risk (HAS-BLED score≥3), triple therapy is recommended for up to 4 weeks, then dual therapy with anticoagulant
and aspirine and clopidogrel for up to one year, then oral anticoagulation for lifetime. For the patient with medical management only the guideline is recommending dual therapy with anticoagulant and aspirine or clopidogrel. 21 Nevertheless, administering triple antithrombotic therapy in elderly patients may have a number of risks, especially concearning bleeding complications. One of the options taken into consideration in order to minimize bleeding risk, emerged after the WOEST trial, is the one that is recommending dual antithrombotic therapy with clopidogrel and anticoagulant as an alternative to triple antithrombotic therapy in patients with great hemoragic risk24. Other strategies recommended in order to minimize bleeding risk in elderly patients that require triple therapy are the use of radial vs. femoral approach, the use of bare-metal stents vs. drug eluting ones and the use of proton pump inhibitors with low inhition of
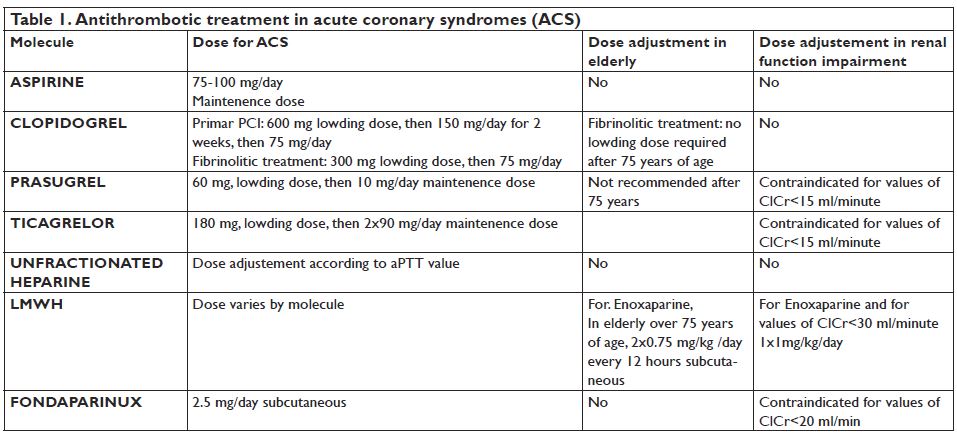
CYPC19 capacity (ex. Pantoprazol)1. Since oral anticoagulation with vitamin K antagonists has a number of limitations such as late therapeutic effect, great interindividual variability of the therapeutic response and multiple drug interactions, the use of new oral anticoagulants in patients with non-valvular atrial fibrilation is nowadays well documented25,26. The use of new oral anticoagulants in the setting of acute coronary syndromes can be a great challenge, especially while treating elderly patients. Among these, three anticoagulant agents are currently available:
dabigatran etexilate, a new direct thrombin inhibitor and rivaroxaban and apixaban, both inhibitors of factor Xa (Table 2). A number of clinical trials have evaluated the efficacy of these agents in the prevention of stroke and systemic embolism in patients with non valvular atrial fibrillation, all these trials demonstrating the non-inferiority of these new anticoagulant agents versus warfarine: dabigatran etexilate – the RE-LY trial (Randomized Evaluation of Long Term Anticoagulant Therapy), rivaroxaban – the ROCKET-AF trial (An Efficacy and Safety Study of Rivaroxaban With Warfarin for the Prevention of Stro ke and Non-Central Nervous System Systemic Embol ism in Patients With Non-Valvular Atrial Fibrillation) and apixaban – the ARISTOTLE trial (Apixaban for the Prevention of Stroke in Subjects With Atrial Fibrillation)27-29. On the other hand, since factor Xa plays a central role in thrombosis, the study ATLAS ACS 2–TIMI 51
(Rivaroxaban in Combination With Aspirin Alone or With Aspirin and a Thienopyridine in Patients With Acute Co ronary Syndromes) has evaluated the efficacy of rivaroxaban administered in small dose (2×2.5 mg/day and 2×5 mg/day) in patients with acute coronary syndrome, in addition to standard therapy. Best results in reducing the rate of cardiovascular death were found with the
2×2.5 mg/day dose, but however the therapy with rivaroxaban was associated with an increased rate of hemorrage30.
CONCLUSIONS
Elderly patients, always between ischemic and hemoragic risk, are requiering a special management of antithrombotic therapy in the setting of acute coronary syndromes, with the need of individualization of therapy for each patient, with close evaluation of the clinical condition.
Conflict of interest: none declared.
References
1. Nichols M, Townsend N, Scarborough P, Rayner M. Cardiovascular disease in Europe: epidemiological update. Eur Heart J 2013;34:3028– 3034.
2. Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, Peto R, Buring J, Hennekens C, Kearney P, Meade T, Patrono C, Roncaglioni MC, Zanchetti A. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomized trials. Lancet 2009; 373:1849–1860.
3. Aronow WS. Approach to symptomatic coronary disease in the elderly: TIME to change? Lancet 2001;358:945–946.
4. Steg PG, Huber K, Andreotti F, Arnesen H, Atar D, Badimon L, Bassand JP, De Caterina R, Eikelboom JA, Gulba D, Hamon M, Helft G, Fox KA, Kristensen SD, Rao SV, Verheugt FW, Widimsky P, Zeymer U, Collet JP. Bleeding in acute coronary syndromes and percutaneous coronary interventions: position paper by the Working Group on Thrombosis of the European Society of Cardiology. Eur Heart J 2011;32:1854 –1864.
5. Mari D, Ogliari G, Castaldi D, Vitale G, Bollini EM, Lio D. Hemostasis and ageing. Immun Ageing 2008;5:12.
6. Laurent S. Defining vascular aging and cardiovascular risk. J Hypertens 2012; 30(suppl.):S3–S8.
7. Karsch-Volk M, Schmid E, Wagenpfeil S, Linde K, Heemann U, Schneider A. Kidney function and clinical recommendations of drug dose adjustment in geriatric patients. BMC Geriatr 2013;13:92.
8. Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, Peto R, Buring J, Hennekens C, Kearney P, Meade T, Patrono C, Roncaglioni MC, Zanchetti A. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 2009; 373:1849–1860.
9. Ikeda Y, Shimada K, Teramoto T, Uchiyama S, Yamazaki T, Oikawa S, Sugawara M, Ando K, Murata M, Yokoyama K, Ishizuka N. Low-dose aspirin for primary prevention of cardiovascular events in Japanese patients 60 years or older with atherosclerotic risk factors: a randomized clinical trial. JAMA 2014;312:2510–2520.
10. Patrono C, Garcia Rodriguez LA, Landolfi R, Baigent C. Low-dose aspirin for the prevention of atherothrombosis. N Engl J Med 2005;353:2373–2383.
11. Andreotti F, Rocca B, Husted S, Ajjan RA, ten Berg J, Cattaneo M, Collet JP, De Caterina R, Fox KA, Halvorsen S, Huber K, Hylek EM, Lip GY, Montalescot G, Morais J, Patrono C, Verheugt FW, Wallentin L, Weiss TW, Storey RF; ESC Thrombosis Working Group. Antithrombotic therapy in the elderly: expert position paper of the European Society of Cardiology Working Group on Thrombosis. Eur Heart J. 2015 Dec 7;36(46):3238-49. doi: 10.1093/eurheartj/ehv304. Epub 2015 Jul 9.
12. Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 2001;345:494–502.
13. Chen ZM, Jiang LX, Chen YP, Xie JX, Pan HC, Peto R, Collins R, Liu LS. Addition of clopidogrel to aspirin in 45,852 patients with acute myocardial infarction: randomised placebo-controlled trial. Lancet 2005;366:1607–1621.
14. Sabatine MS, Morrow DA, Montalescot G, Dellborg M, Leiva-Pons JL, Keltai M, Murphy SA, McCabe CH, Gibson CM, Cannon CP, Antman EM, Braunwald E. Angiographic and clinical outcomes in patients receiving low-molecular-weight heparin versus unfractionated heparin in ST-elevation myocardial infarction treated with fibrinolytics in the CLARITY-TIMI 28 trial. Circulation 2005;112: 3846–3854.
15. Mauri L, Kereiakes DJ, Yeh RW, Driscoll-Shempp P, Cutlip DE, Steg PG, Normand SL, Braunwald E, Wiviott SD, Cohen DJ, Holmes DR Jr, Krucoff MW, Hermiller J, Dauerman HL, Simon DI, Kandzari DE, Garratt KN, Lee DP, Pow TK, Ver Lee P, Rinaldi MJ, Massaro JM. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med 2014;371:2155–2166.
16. Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, Neumann FJ, Ardissino D, De Servi S, Murphy SA, Riesmeyer J, Weerakkody G, Gibson CM, Antman EM. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2007;357:2001–2015.
17. Husted S, James S, Becker RC, Horrow J, Katus H, Storey RF, Cannon CP, Heras M, Lopes RD, Morais J, Mahaffey KW, Bach RG, Wojdyla D, Wallentin L. Ticagrelor versus clopidogrel in elderly patients with acute coronary syndromes: a substudy from the prospective randomized PLATelet Inhibition and Patient Outcomes (PLATO) trial. Circ Cardiovasc Qual Outcomes 2012;5:680–688.
18. Mauri L, Kereiakes DJ, Yeh RW, Driscoll-Shempp P, Cutlip DE, Steg PG,Normand SL, Braunwald E, Wiviott SD, Cohen DJ, Holmes DR Jr,Krucoff MW, Hermiller J, Dauerman HL, Simon DI, Kandzari DE, Garratt KN, Lee DP, Pow TK, Ver Lee P, Rinaldi MJ, Massaro JM. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med 2014;371:2155–2166.
19. Steg PG, James SK, Atar D, Badano LP, Lundqvist CB, Borger MA, Di Mario C, Dickstein K, Ducrocq G, Fernandez-Aviles F, Gershlick AH, Giannuzzi P, Halvorsen S, Huber K, Juni P, Kastrati A, Knuuti J, Lenzen MJ, Mahaffey KW,Valgimigli M, van’t Hof A, Widimsky P, Zahger D. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). Eur Heart J 2012;33:2569–2619.
20. Schiele F. Fondaparinux and acute coronary syndromes: update on the OASIS 5–6 studies. Vasc Health Risk Manag 2010;6:179–187.
21. Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, Bax JJ, Borger MA, Brotons C, Chew DP, Gencer B, Hasenfuss G, Kjeldsen K, Lancellotti P, Landmesser U, Mehilli J, Mukherjee D, Storey RF, Windecker S, Baumgartner H, Gaemperli O, Achenbach S, Agewall S, Badimon L, Baigent C, Bueno H, Bugiardini R, Carerj S, Casselman F, Cuisset T, Erol Ç, Fitzsimons D, Halle M, Hamm C, Hildick-Smith D, Huber K, Iliodromitis E, James S, Lewis BS, Lip GY, Piepoli MF, Richter D, Rosemann T, Sechtem U, Steg PG, Vrints C, Luis Zamorano J. 2015
ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016 Jan 14;37(3):267-315. doi: 10.1093/eurheartj/ehv320. Epub 2015 Aug 29.
22. Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, Hindricks G, Kirchhof P. ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fi brillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012;33:2719-47.
23. Task Force Members, Lip GY, Windecker S, Huber K, Kirchhof P, Marin F, Ten Berg JM, Haeusler KG, Boriani G, Capodanno D, Gilard M, Zeymer U, Lane D, Storey RF, Bueno H, Collet JP, Fauchier L, Halvorsen S, Lettino M, Morais J, Mueller C, Potpara TS, Rasmussen LH, Rubboli A, Tamargo J, Valgimigli M, Zamorano JL. Management of antithrombotic therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous coronary or valve interventions: a joint consensus document of the Euro pean Society
of Cardiology Working Group on Thrombosis, Euro pean Heart Rhythm Association (EHRA), European Association of Percu taneous Cardiovascular Interventions (EAPCI) and European Asso ciation of Acute Cardiac Care (ACCA) endorsed by the Heart Rhythm Society (HRS) and Asia-Pacifi c Heart Rhythm Society (APHRS). Eur Heart J. 2014;35:3155-79.
24. Dewilde WJ, Oirbans T, Verheugt FW, Kelder JC, De Smet BJ, Herrman JP, Adriaenssens T, Vrolix M, Heestermans AA, Vis MM, Tijsen JG, van ‘t Hof AW, ten Berg JM; WOEST study investigators. Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: an open-label,
randomised, controlled trial. Lancet. 2013;381:1107-15.
25. Mihaela Rugină, Mihaela Sălăgean, L. Predescu, E. Apetrei. Noi anticoagulante orale. Romanian Journal of Cardiology Vol. 22, No. 1, 2012.
26. Carmen Ginghină, Elena-Laura Antohi, Ruxandra Jurcuţ, Laura Dima. Particularităţi ale tratamentului antitrombotic la pacientul vârstnic. Romanian Journal of Cardiology Vol. 21, No. 3, 2011.
27. Ezekowitz MD, Connolly S, Parekh A, Reilly PA, Varrone J, Wang S, Oldgren J, Themeles E, Wallentin L, Yusuf S. Rationale and design of RE-LY: randomized evaluation of long-term anticoagulant therapy, warfarin, compared with dabigatran. Am Heart J. 2009;157:805– 810.
28. Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, et all; ROCKET AF Investigators. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011 Sep 8;365(10):883-91.
29. Connolly SJ, Eikelboom J, Joyner C, et al. Apixaban in patients with atrial fi brillation. N Engl J Med 2011;364:806-17.
30. Mega JL, Braunwald E, Wiviott SD, Bassand JP, et all; ATLAS ACS 2– TIMI 51 Investigators. Rivaroxaban in patients with a recent acute coronary syndrome, N Engl J Med. 2012 Jan 5;366(1):9-19.
 This work is licensed under a
This work is licensed under a