Irina Pintilie1, Mihaela Ispas1, Ayman Elkahlout1, Alina Scridon2,3, Razvan Constantin Serban1,2, Dan Dobreanu1,2
1 Emergency Institute for Cardiovascular Diseases and Transplantation, Tirgu Mures, Romania
2 University of Medicine and Pharmacy, Tirgu Mures, Romania
3 Center for Advanced Medical and Pharmaceutical Research, Tirgu Mures, Romania
Abstract: Introduction – Acute coronary syndromes are rare in heart transplant recipients. They are usually linked to cardiac allograft vasculopathy, one of the main complications of heart transplantation, characterized by early and rapidly progressing arteriosclerosis. Case presentation – We report the case of a 58-year-old female who underwent heart transplantation at the age of 44 years. The patient presented at the Emergency Department 24 h after the onset of unspecific symptoms (epigastric discomfort, fatigue, general weakness). A diagnosis of ST-segment elevation myocardial infarction was established based on the electrocardiogram and the increased levels of cardiac necrosis markers. Coronary angiogram revealed proximal occlusion of the right coronary artery, with no other atherosclerotic lesions. A drug-eluting stent was implanted, with good angiographic result. Post-angioplasty, the clinical course was uneventful. Conclusion – Acute myocardial infarction is a rare, but serious complication in heart transplant recipients. Symptoms can be misleading in this subgroup of patients and a careful evaluation of new symptoms should always be made. Although acute coronary syndromes are usually due to cardiac allograft vasculopathy, in our case, the presence of a single, focal coronary lesion of a proximal vessel at more than 14 years after heart transplant suggests typical atherosclerosis of the transplanted heart.
Keywords: heart transplant, cardiac allograft vasculopathy, STEMI
INTRODUCTION
Heart transplantation (HTx) is a life-saving procedure and the gold standard treatment for end-stage heart failure. However, the number of heart transplants is in decline, mainly due to the scarcity of donor organs1. Acute coronary syndromes (ACS) in HTx recipients are uncommon. Furthermore, due to cardiac denervation, initial presentation is usually atypical, with symptoms
that may often be misleading2. Cardiac allograft vasculopathy (CAV), defi ned as early development of rapidly progressing coronary artery disease in the transplanted heart, represents one of the most important long-term complications of HTx and a major cause of morbidity and mortality in this subgroup of patients3. Allograft vasculopathy is characterized by an accelerated and diffuse process of arteriosclerosis, occurring in about 50% of patients at 5 years from transplantation4. Differentiating CAV from typical athe rosclerosis can sometimes be difficult in clinical practice, although criteria have been published more than 10 years ago5.
CASE REPORT
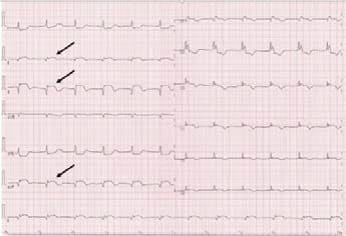
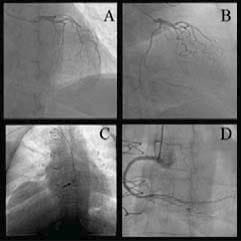
We present the case of a 58-year-old female who underwent HTx for end-stage heart failure secondary to ischemic dilated cardiomyopathy 14 years before. The patient first presented to her family physician for epigastric discomfort accompanied by intense fatigue, dizziness, and generalized weakness. She was prescribed antacids and no further investigations were performed. Due to persistence of symptoms, the patient presented the next day to the Emergency Department of our hospital, approximately 24 hours after symptoms onset. Her medical history included arterial hypertension, obesity, and dyslipidemia. The patient was on long-term therapy with immunosuppressive agents (cyclosporine and mycophenolate mofetil), cotrimoxazole, calcium channel blocker, loop and mineralocorticoid antagonist diuretics, and a statin. Physical examination showed a body mass index of 37.1 kg/m2 and a heart rate of 70 beats per minute; her blood pressure was 110/90 mmHg; cardiac and pulmonary examinations were unremarkable. The electrocardiogram (Figure 1) revealed normal sinus rhythm with right bundle branch block (already known), STsegment elevation in the inferior leads, alongside with pathological Q waves in the same territory, and depressed ST-segment in leads I and aVL, with inverted T waves in leads V3 to V6. Cardiac necrosis biomarkers showed elevated troponin I (27.1 ng/ml), creatin kinase (3.000 IU/l), and creatin-kinase myocardial band (236 IU/l) levels. Transthoracic echocardiogram revealed hypokinesia of the left ventricular inferior wall, with a preserved left ventricular ejection fraction of 45%, grade I diastolic dysfunction, and moderate mitral regurgitation. Based on these findings, the patient was diagnosed with acute inferior ST-segment elevation myocardial infarction (STEMI), and treated, according to current practice guidelines, with dual antiplatelet therapy (DAPT), low-weight molecular heparin, statin, and beta-blocker. Coronary angiogram revealed no atherosclerotic lesions of the left coronary artery (Figure 2 A and B), and proximal occlusion of the right coronary artery as culprit lesion (Figure 2 C). A drug-eluting stent was successfully implanted at the site of the lesion (Figure 2 D). The patient was discharged seven days later, after an uneventful evolution.
Figure 1. Twelve-lead electrocardiogram showing normal sinus rhythm, with fl at P waves and prolonged PQ interval (220 ms), ST-segment elevation in leads II, III, and aVF (arrows), pathological Q waves in the same territory, and complete right bundle branch block with secondary repolarization abnormalities.
Figure 2. Coronary angiogram. Left coronary artery in right anterior oblique cranial view (A) and right anterior oblique caudal view (B). Complete occlusion of the right coronary artery (arrow) in left anterior oblique view (C), and opening of the artery after stent deployment in left anterior oblique view (D).
DISCUSSIONS
As the transplanted heart remains denervated over time, this subgroup of patients is lacking the typical symptoms of myocardial ischemia, making the diagnosis of ACS a real challenge. In a series of cases of acute myocardial infarction (AMI) in HTx recipients, only three out of 25 patients experienced typical chest or arm pain6. The initial symptoms mainly consisted of dyspnea, fatigue, weakness, palpitations, dizziness, nausea, or diaphoresis. Only nine out of those 25 patients were admitted to hospital with an initial diagnosis of AMI, the rest being diagnosed either at the time of coronary angiography or at autopsy. Similarly, the initial presentation of our patient, with unspecific symptoms, was misleading and delayed the patient’s presentation to a percutaneous coronary intervention center. For an early detection of acute ischemia in this subgroup of patients, a high index of suspicion is therefore mandatory. The underlying mechanism of STEMI in this patient may be related to either the initial atherosclerosis process, now affecting the transplanted heart, or to a late expression of CAV. Cardiac allograft vasculopathy has many similarities with native atherosclerotic disease; however, major differences have been shown to exist between the two conditions. From a pathophysiological point of view, CAV is initiated by intensive smooth muscle cells proliferation in the intima of the vessels and it may appear as early as 1 week or 2 weeks after transplantation, followed by accelerated progression of the disease. This process affects both the epicardial and the intramural vessels, but also the cardiac veins, resulting in diffuse vessel involvement. Meanwhile, typical atherosclerosis affects mainly the proximal epicardial coronary arteries. Also, whereas CAV typically consists of concentric and diffuse intimal thickening, leading to extended vessel narrowing7,8, typical atherosclerosis usually causes multiple, focal, eccentric lesions of the intima. Despite their different manifestations, typical atherosclerosis and CAV share common risk factors. The onset and development of both CAV and typical atherosclerosis are triggered by factors such as hyperlipidemia, diabetes mellitus, arterial hypertension, infections, inflammation, and smoking. On the other hand, factors such as ischemia/reperfusion graft injury, cytomegalovirus infection, and HLAdirected antibodies were shown to interfere only with CAV progression9,10. In clinical practice, the diagnosis of CAV relies on both coronary angiography (i.e., diffuse lesions of the epicardial coronary arteries) and echocardiography (impaired left ventricular ejection fraction, restrictive profile of the left ventricular diastolic function) data11,12. Other modern imaging techniques have also proved useful for CAV diagnosis. Intravascular ultrasound can detect and quantify the early signs of intimal thickening13,14, being proposed by the International Society for Heart and Lung Transplantation as surrogate marker for prognosis. Optical coherence tomography can diagnose and detect vulnerable plaques and complicated coronary lesions15, whereas contrast echocardiography can assess the microcirculation by measuring the coronary fl ow reserve (CFR), reduced CFR being an early marker of CAV16. Unfortunately, none of these techniques were used in our case, limiting our ability to distinguish with certainty between CAV and atherosclerosis. Evaluation of CAV biomarkers would also have been of interest. Indeed, several markers have been tested in this regard, from soluble interleukin-2 receptors17, to cell type ratios18, and, more recently, to microRNAs19. However, none of these markers has imposed so far in clinical practice. According to the recommendations of the International Society for Heart and Lung Transplantation, a diagnosis of CAV can be established based solely on coronary angiography and echocardiography parameters5. In our patient, repeated coronary angiography and echocardiographic assessment at 1, 2, and 3 years post-HTx excluded the presence of de novo coronary atherosclerosis and of CAV. The patient remained completely asymptomatic until the occurrence of the present STEMI, making it difficult to distinguish with certainty between typical coronary atherosclerosis and late-onset CAV. However, the finding of single-vessel involvement, the presence of a focal lesion in only one of the major epicardial coronary arteries, together with the absence of impaired left ventricular ejection fraction and of a restrictive profile of the left ventricular diastolic function, may be interpreted as signs of systemic atherosclerotic disease rather than CAV, as previously suggested by Fazio et al20. However, given the scarcity of such cases, it remains difficult to draw a fi rm conclusion. Adequate differentiation between typical atherosclerosis and CAV may have important therapeutic impact, given that although both CAV and de novo atherosclerosis could beneficiate from percutaneous coronary interventions or coronary artery bypass-graft21,22, the most effective therapy in severe CAV cases remains cardiac re-transplantation23. According to the current guidelines regarding the management of patients presenting with STEMI24, DAPT will be continued for up to 12 months in our patient. The role of aspirin after heart transplantation has been controversial25, recent data suggesting it may reduce the risk of CAV and mortality in HTx patients26. In our case, considering the presence of an ACS in a heart transplant recipient, aspirin will be continued lifelong. In addition to aspirin, statins are also well known to influence short-term and long-term prognosis in this subset of patients by reducing cholesterol levels, improving endothelial dysfunction, and having anti-inflammatory activity27; accordingly, lifelong statin therapy was also prescribed. Although our patient can be considered at very high risk of complications, there are no data so far to recommend more aggressive therapies, such as lifelong DAPT or association of DAPT with oral anticoagulation. Adequate treatment of AMI in our patient will also have to be followed by a very close follow-up, given that late development of an atherosclerotic lesion in an HTx recipient appears to trigger rapid atherosclerosis progression28. Conclusion: Acute myocardial infarction is a rare, but serious complication in HTx recipients. Symptoms can be misleading in this subgroup of patients; the onset of any possibly cardiac-related new symptoms should lead to careful examination and exclusion of ischemic events. Although ACS are usually due to CAV, in our case, the presence of a single, focal coronary lesion of a proximal vessel, at more than 14 years after HTx, suggests typical atherosclerosis of the transplanted heart.
Funding: This work was supported by the University of Medicine and Pharmacy of Tirgu Mures Research Grant number 17800/1/22.12.2015.
Conflicts of interest: none declared.
References
1. Komadja M, Ruschitzka F. The year in cardiology 2015: heart failure. Romanian Journal of Cardiology, 2016;26: 128-32.
2. Peter S, Hulme O, Deuse T, Vrtovec B, Fearon WF, Hunt S, Haddad F. ST-elevation myocardial infarction following heart transplantation as an unusual presentation of coronary allograft vasculopathy: a case report. Transplant Proc 2013;45: 787-91.
3. Segura AM, Buja LM. Cardiac allograft vasculopathy. Tex Heart Inst J 2013;40: 400-2.
4. Stehlik J, Edwards LB, Kucheryavaya AY, Aurora P, Christie JD, Kirk R Rahmel AO, Stehlik J, Hertz MI. The Registry of the International Society for Heart and Lung Transplantation: twenty-seventh offi cial adult heart transplant report–2010. J Heart Lung Transplant 2010;29: 1089-103.
5. Mehra MR, Crespo-Leiro MG, Dipchand A, Ensminger SM, Hiemann NE, Kobashigawa JA, Madsen J, Parameshwar J, Starling RC, Uber PA. International Society for Heart and Lung Transplantation working formulation of a standardized nomenclature for cardiac allograft vasculopathy – 2010. J Heart Lung Transplant 2010;29: 717-27.
6. Gao SZ, Schroeder JS, Hunt SA, Billingham ME, Valantine HA, Stinson EB. Acute myocardial infarction in cardiac transplant recipients. Am J Cardiol 1989;64: 1093-7.
7. Insull W, Jr. The pathology of atherosclerotic plaque development and plaque responses to medical treatment. Am J Med 2009;122: S3-14.
8. Rahmani M, Cruz RP, Granville DJ, McManus BM. Allograft vasculopathy versus atherosclerosis. Circ Res 2006;99: 801-15.
9. Delgado JF, Reyne AG, de Dios S, López-Medrano F, Jurado A, Juan RS, RuizCano MJ, Dolores Folgueira M, Gómez-Sánchez MÁ, Aguado JM, Lumbreras C. Infl uence of cytomegalovirus infection in the development of cardiac allograft vasculopathy after heart transplantation. J Heart Lung Transplant 2015;34:1112-9.
10. Pober JS, Jane-Wit D, Qin L, Tellides G. Interacting mechanisms in the pathogenesis of cardiac allograft vasculopathy. Arterioscler Thromb Vasc Biol 2014;34: 1609-14.
11. St Goar FG, Pinto FJ, Alderman EL, Valantine HA, Schroeder JS, Gao SZ, Stinson EB, Popp RL. Intracoronary ultrasound in cardiac transplant recipients. In vivo evidence of” angiographically silent” intimal thickening. Circulation 1992;85: 979-87.
12. Javaheri A, Saha N, Lilly SM. How to approach the assessment of cardiac allograft vasculopathy in the modern era: review of invasive imaging modalities. Curr Heart Fail Rep 2016;13: 86-91.
13. Tuzcu EM, Kapadia SR, Sachar R, Ziada KM, Crowe TD, Feng J, Magyar WA, Hobbs RE, Starling RC, Young JB, McCarthy P. Intravascular ultrasound evidence of angiographically silent progression in coronary atherosclerosis predicts long-term morbidity and mortality after cardiac transplantation. J Am Coll Cardiol 2005;45: 1538-42.
14. Kobashigawa JA, Tobis JM, Starling RC, Tuzcu EM, Smith AL, Valantine HA, Yeung AC, Mehra MR, Anzai H, Oeser BT, Abeywickrama KH. Multicenter intravascular ultrasound validation study among heart transplant recipients: outcomes after fi ve years. J Am Coll Cardiol 2005;45: 1532-7.
15. Cassar A, Matsuo Y, Herrmann J, et al. Coronary atherosclerosis with vulnerable plaque and complicated lesions in transplant recipients: new insight into cardiac allograft vasculopathy by optical coherence tomography. Eur Heart J 2013;34(33):2610-2617
16. Tona F, Osto E, Famoso G, Previato M, Fedrigo M, Vecchiati A, Perazzolo Marra M, Tellatin S, Bellu R, Tarantini G, Feltrin G. Coronary microvascular dysfunction correlates with the new onset of cardiac allograft vasculopathy in heart transplant patients with normal coronary angiography. Am J Transplant 2015;15: 1400-6.
17. Young JB, Windsor NT, Kleiman NS, Lowry R, Cocanougher B, Lawrence EC. The relationship of soluble interleukin-2 receptor levels to allograft arteriopathy after heart transplantation. J Heart Lung Transplant 1992;11(3 Pt 2): S79-82.
18. Roldán C, Mirabet S, Cecilia C, Brossa V, Roig E, Martín C, Gelpí C. CD4 + CD45RO + CD25-/lowCD127+: CD4 + CD45RO + CD25hiCD127-/low ratio in peripheral blood: a useful biomarker to detect cardiac allograft vasculopathy in heart transplanted patients. Transplantation 2015;99: 1521-8.
19. Neumann A, Napp LC, Kleeberger JA, Benecke N, Pfanne A, Haverich A, Thum T, Bara C. MicroRNA 628-5p as a novel biomarker for cardiac allograft vasculopathy. Transplantation 2017;101:e26-33.
20. Fazio G, Sutera L, Vernuccio D, Fazio M, Novo S. Symptomatic acute myocardial infarction in a patient bearer of heart transplantation following ischemic heart disease. Int J Cardiol 2008;124: 233-6
21. Musci M, Loebe M, Wellnhofer E, Meyer R, Pasic M, Hummel M, Bocksch W, Grauhan O, Weng Y, Hetzer R. Coronary angioplasty, bypass surgery, and retransplantation in cardiac transplant patients with graft coronary disease. Thorac Cardiovasc Surg 1998;46: 268-74.
22. Aqel RA, Wells BJ, Hage FG, Tallaj J, Benza R, Pamboukian S, Rayburn B, McGiffi n D, Kirklin J, Bourge R. Re-stenosis after drug-eluting stents in cardiac allograft vasculopathy. J Heart Lung Transplant 2008;27: 610-5.
23. Johnson MR, Aaronson KD, Canter CE, Kirklin JK, Mancini DM, Mehra MR, Radovancevic B, Taylor DO, Webber SA. Heart retransplantation. Am J Transplant 2007;7: 2075-81.
24. Steg G, James SK, Atar D et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). Eur Heart J 2012;30:2597-9.
25. Costanzo MR, Dipchand A, Starling R, et al. The International Society of Heart and Lung Transplantation Guidelines for the care of heart transplant recipients. J Heart Lung Transplant. 2010;29:914-56.
26. Peled, Y. et al. Early Aspirin Initiation Following Heart Transplantation Decreases the Risk of Allograft Vasculopathy During Long-Term Follow. J Heart Lung Transplant. 2017:36:142.
27. Szyguła-Jurkiewicz B, Szczurek W, Zembala M. The role of statins in patients after heart transplantation. Kardiochir Torakochirurgia Pol 2015;12:42-47.
28. Shah P, Bajaj S, Virk H, Bikkina M, Shamoon F. Rapid progression of coronary atherosclerosis: a review. Thrombosis 2015;2015: 634983.
 This work is licensed under a
This work is licensed under a