Lucica Grigorică1, C. Macarie2
Article received on the 21st of March 2012. Article accepted on the 12th of August 2012.
1 “Saint Andrew” Emergency Clinical Hospital, Galati
2 “Prof. Dr. C.C. Iliescu” Emergency Institute for Cardiovascular Diseases, Bucharest
Prof. Dr. Cezar Macarie, “Prof. Dr. C.C. Iliescu” Emergency Institute for Cardiovascular Diseases, 258 Fundeni Str., Sector 2, Bucharest, Post Code – 022328. Tel.: 0213180400.
Dr. Lucica Grigorică – luci22grigorica@yahoo.com
Abstract: Acute heart failure has become a real public health issue in the USA, as well as in many European countries. Mortality rates during hospitalization remain high. Clinical trials have yet to prove their efficiency in generating therapies capable of improving survival rates. The authors of this observational study have enrolled in the study randomly selected patients, chosen from two hospitals of different ranking and analyzed the demographical, evolution, clinical and treatment characteristics. The following independent negative predictors were identified by using a multivariate regression logistic model: arterial hypotension, renal dysfunction, peripheral edema, anemia and severe left ventricle systolic dysfunction. In contrast, high blood pressure at admission and the use of beta-blockers during admission were protection factors, being associated with a positive prognostic.
Keywords: acute heart failure, prognostic factors
Rezumat: Insuficienţa cardiacă acută a devenit în SUA şi în multe ţări europene o reală problemă de sănătate publică. Mortalitatea acestor pacienţi pe perioada internării rămâne în continuare crescută. Trialurile clinice nu şi-au dovedit utilitatea în generarea de terapii care să amelioreze supravieţuirea. Autorii acestui studiu observațional au înrolat pacienţi neselecţionaţi din două spitale de rang diferit şi au analizat caracteristicile demografice, clinice, evolutive şi de tratament. Utilizând un model logistic de regresie multivariată au fost evidenţiaţi următorii predictori independenţi de prognostic negativ: hipotensiunea arterială, disfuncţia renală, edemele periferice, anemia şi disfuncţia sistolică severă de ventricul stâng. În contrast, tensiunea arterială crescută la internare şi utilizarea beta blocantelor pe perioada internării au fost factori de protecţie care s-au asociat cu un prognostic pozitiv.
Cuvinte cheie: insuficienţa cardiacă acută, factori de prognostic
“The very essence of cardiovascular practice is the early detection of heart failure…”
Sir Thomas Lewis, 1933
Introduction
Patients suffering from acute heart failure (HF) have increased mortality rates during hospitalization, but this tendency is also present after they are discharged. In addition, they also have high re-admission rates. The key to improving these patients’ prognostic is to fully understand the complexity and the heterogeneity of the acute heart failure syndrome. The current data on acute heart failure was offered by clinical trials and acute HF registries. The rigid and exclusive selection criteria used for clinical trials have not permitted a selection of patients representative for “the real world”. In this context, elders, patients with numerous comorbidities, severe forms of acute HF and patients with a well preserved ejection fraction were often excluded from trials. As opposed to clinical trials, registries have an “all inclusive” character – reflecting the “real world” of patients suffering from acute HF. The enrolment of randomly picked patients allows us to obtain essential information about the demographical, clinical and management characteristics of these patients, as well as prognostic data.
OBJECTIVE
The authors of this study set out to identify the negative prognostic factors during hospitalization within a cohort of patients admitted for acute HF as their main diagnostic.
MATERIALS AND METHODS
The study included a cohort comprised of two lots of patients, consecutively admitted, diagnosed with acute HF in two different hospitals of different ranking: an academic hospital (the 1st Cardiology Unit – “Prof.Dr. C.C. Iliescu” Emergency Institute for Cardiovascular Diseases, Bucharest) and a non-academic hospital (the Cardiology Unit – “Saint Andrew” Emergency Clinical Hospital, Galaţi). The enrollment period was between the 1st of January and the 31st of December 2007. Only patients with acute HF were included. The patients were categorized into the following clinical forms: chronic decompensated HF, acute pulmonary edema (APE), cardiogenic shock, acute HF in hypertension peaks and isolated acute right HF. This classification was done in accordance with the recommendations of the European Society of Cardiology regarding the diagnosis and treatment of acute and chronic heart failure from 20081.
STATISTICAL ANALYSIS OF THE DATA
All the data (consisting of demographical information, medical history, evolution, treatment and health status at discharge) was integrated in an electronic questionnaire which was filled out during the hospitalization. The collected data was introduced in an Excel data base. The quality of the data was randomly checked. The data analysis was performed by using SPSS version 17 and Open Epi. The relevance threshold was considered at 95% and the difference was deemed statistically relevant when the value of p was <0.05%.
RESULTS
General data
The studied cohort consisted of 424 patients: 221 were enrolled in the academic hospital unit and 203 were recruited in the non-academic hospital. The mean age of the studied lot was 66.44 ±12.45 years, with a predominance of male patients (63.4%). Decompensated chronic HF was the clinical form most often diagnosed (69.8%), followed by APE and cardiogenic shock (Figure 1).
Acute de novo HF was diagnosed in 18.65% of the cases. Compared to decompensated chronic HF, the “de novo” form was characterized by an increased frequency of severe acute HF (1/3 of these patients presented cardiogenic shock or APE on admission).
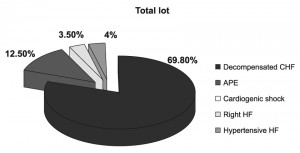
Figure 1. Patient’s clinical profile on admission into the hospital.
By analyzing the medical history of the patients included in the study we realized that 40% of the patients presented angina pectoris and/or myocardial infarction, approximately one third suffered from diabetes, 12% suffered a stroke, 8.3% presented chronic peripheral arteriopathy, 14.6% suffered from chronic kidney disease and 9% had chronic obstructive bronchopneumopathy.
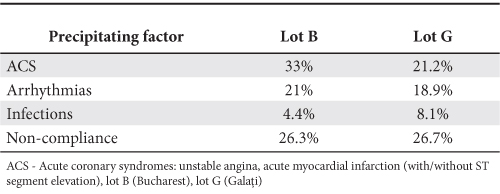
In the cohort we studied the predominant etiology of HF was ischemia (55.9%), followed by valve conditions (14.8% in the lot from Bucharest and 10.8% in the one from Galaţi). The most frequent precipitating factors were: myocardial ischemia, arrhythmias, infections and lack of compliancy to the drug therapy and low/sodium free diet, with small differences between the two hospitals (Table 1). It is important to mention that acute coronary syndromes were the main precipitating factor for an overwhelming majority of the cases with cardiogenic shock (81.8% the Galaţi lot vs 71.7% the Bucharest lot, p<0.05) and acute pulmonary edema (46.9% the Galaţi lot vs 38.1% the Bucharest lot, p<0.05).
Table 1. Precipitating factors for acute HF episodes in the study centers
Clinical evaluation
The clinical state of patients suffering from acute HF was dominated by pulmonary or mixed peripheral congestion 76.7% of the patients presented stasis rales, 66% had turgescent jugular veins, 48.6% presented calf edema and 10.1% were found with pleurisy. The physical examination revealed a left ventricle protodiastolic gallop.
Arterial blood pressure is the most important parameter of the on-admission hemodynamic evaluation. The mean values of the sBP (systolic blood pressure) and dBP (diastolic blood pressure) were 134.86±35.05 mmHg, respectively 77.61±18.94 mmHg. The highest BP values were noted for patients with APE in both hospitals, whereas the lowest values were observed in patients in cardiogenic shock. The differences between the two forms of acute HF were statistically significant (p <0.05). The majority of patients had a sBP >90 mmHg upon admission and only 5.4% had a systolic BP <90 mmHg in both lots. Atrial fibrillation was the most common arrhythmia diagnosed in the study lot (35.8% of the patients). The clinical forms which registered the highest prevalence for atrial fibrillation were (for both lots) decompensated chronic HF (47.8%) and acute right HF (40% of the cases). Cardiogenic shock, the most severe form of acute HF, registered the lowest prevalence for atrial fibrillation (22.7%). Compared to decompensated chronic HF, acute de novo HF registered a much lower rate of cases associated with atrial fibrillation (de novo HF – 26.4% vs decompensated chronic HF – 40.5%, p<0.05).
Paraclinical examination
An electrocardiogram was performed on all the patients upon admission. We discovered that left bundle branch block was present at 18.1% of the patients from Bucharest, whilst 19% of the patients from Galaţi presented the same condition. An on-admission echocardiography was performed on 396 of the patients. We noted a predominance of a left ventricle systolic dysfunction in the general lot of study (62.3%of the cases). We considered a left ventricle systolic dysfunction for an ejection fraction of less than 45%. In 30.2% of the cases we found a moderate – severe mitral insufficiency, 5% presented a tight aortic stenosis and 3.5% of the cases presented a moderate – severe aortic insufficiency. Approximately 23% of the patients had moderate – severe pulmonary hypertension upon admission. A cardio-pulmonary X-ray examination was also performed on admission on 385 of the patients from the two hospitals. Around 1/3 of the patients presented cardiomegaly (cardiothoracic index >0.5) and approximately 1/3 suffered from pulmonary congestion. 18.6% of the patients had a normal X-ray.
Biological data
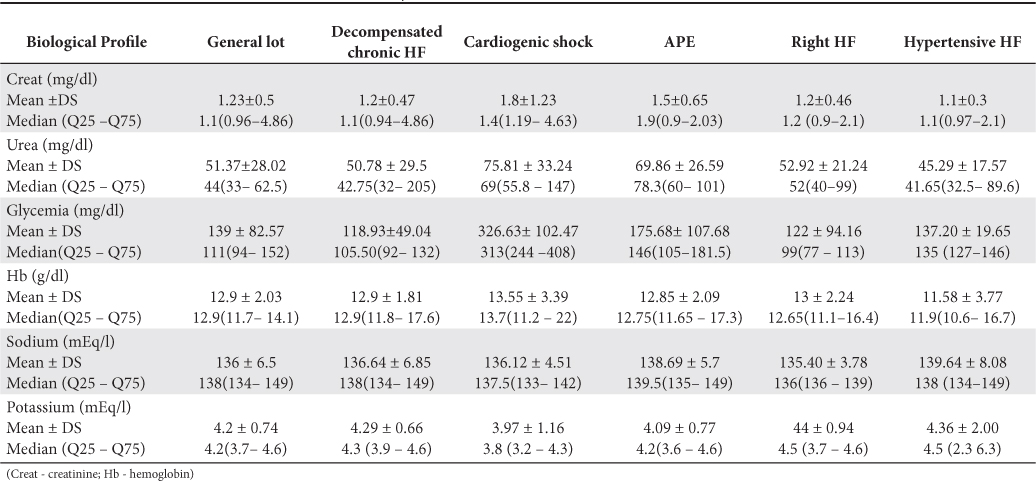
A series of laboratory tests were performed both on admission and at discharge: serum hemoglobin, fasting blood glucose, serum urea, serum creatinine, serum ionogram (sodium and potassium). The mean values of these biological parameters are presented in Tables 1 and 2.
Modified values of the biological parameters were found in severe forms of acute HF. The most severe alteration of the renal function was found in patients in cardiogenic shock, followed by those with acute pulmonary edema. In the lot from Galaţi the mean value of the blood glucose for patients in cardiogenic shock draws attention. Trying to explain this situation we noticed that over 50% of the patients admitted in this hospital in cardiogenic shock had a history of diabetes. In this group, the values of the blood glucose determined on admission varied between 195 and 525 mg/dl, significantly higher when compared to those of the Bucharest group (Tables 2 and 3).
Table 2. Laboratory work-up (values measured on admission) for the Bucharest lot (data available for 208 patients)
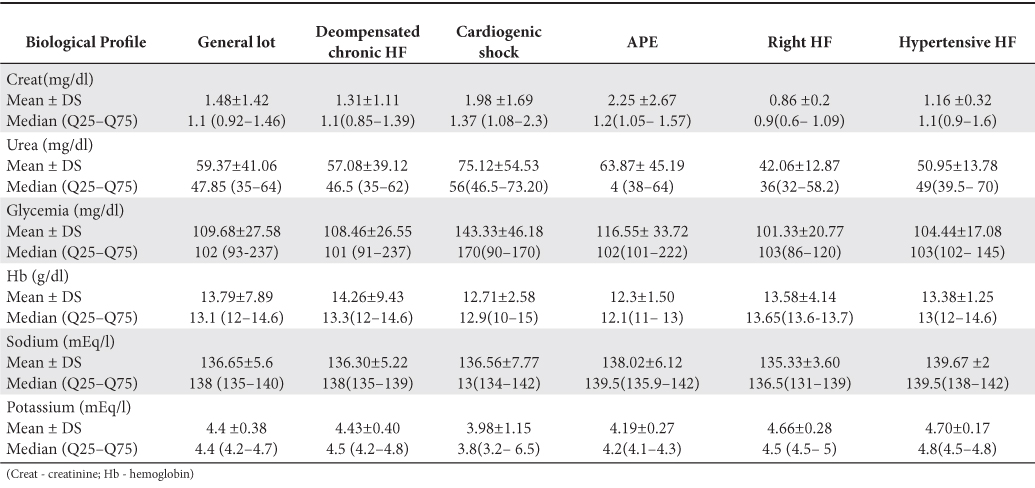
Table 3. Biological profile for the patients in the Galaţi lot (data available for 202 patients)
Treatment
Approximately one quarter of the patients (24.5%) could not remember the treatment they were following at home at the moment of admission and almost one third of the patients (29.2%) were not treating their condition. For the group of patients which were already on a treatment, it was noted that 25% were on beta-blockers, 21.5% were taking loop diuretics and 19.6% were under CEI (converting enzyme inhibitors) (Figure 2). We noticed a low use of medication with a positive impact on survival rates (CEI, beta-blockers and antialdosteronic medication), considering that 80% of the patients were diagnosed with chronic HF.
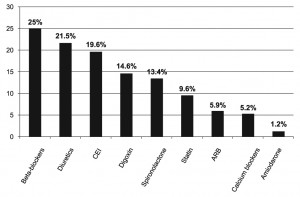
Figure 2. Treatment administered prior to admission (in the general lot) – for the patients undergoing treatment.
On admission, loop diuretics (furosemide) represented the first line of therapy, recommended in both lots for the majority of patients (84.7% of the general lot). We noticed that less than one third of the patients required parenteral administration of nitroglycerine and 16% required positive inotropic medication (Figure 3). For approximately half of the patients from both lots (47.16%) furosemide was the only cardiologic medication administered parenterally.
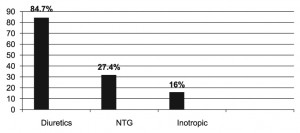
Figure 3. Parenteral treatment administered on admission: data from the general lot (NTG – nitroglycerine).
The oral treatment recommended during admission and upon discharge is presented in Figures 4 and 5.
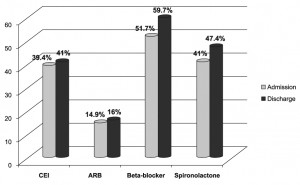
Figure 4. Oral treatment recommended during hospitalization and on discharge (general lot) CEI – converting enzyme inhibitor; ARB – angiotensin II receptors blocker.
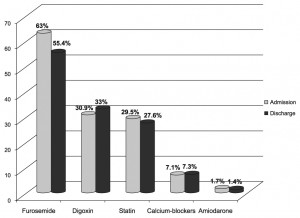
Figure 5. Oral treatment recommended during admission and on discharge (general lot).
During admission, as well as after the patient was discharged from the hospital, the most widely recommended medication remains the loop diuretic. The use of CEI/ARB (converting enzyme inhibitors/angiotensin II receptor blockers), beta-blockers and spironolactone, drugs which have proven to be useful in the increase of survival rates of patients with chronic HF in numerous studies, was very low in the studied cohort. Thus, during admission a little over 50% of the patients received beta-blockers and CEI/BRA and just over 40% received spironolactone. Around 1/3 of the patients were prescribed digoxin in the therapeutic scheme recommended at discharge (Figures 3 and 4). 38.5% of the patients from the general lot which also presented an EF <45% received digitalis, compared to only 10.7% of the patients with a preserved left ventricle ejection fraction.
Although revascularization procedures increase survival rates for patients who have suffered acute coronary syndromes, these procedures are seldom used in acute HF. Despite the development of invasive interventional techniques or surgical myocardial revascularization procedures which are successfully used to help coronary patients, the percentage of patients suffering from acute HF benefiting from these procedures is very low. The records used to gather data regarding this situation show that only 2% of these patients benefit from a revascularization procedure during the same admission in the hospital unit. In the studied cohort, only patients from the Bucharest lot benefited from an emergency angiographic evaluation and possible myocardial revascularization procedures. From 221 patients only 35 (15.83%) were evaluated through a coronarography. Stent placement coronary angioplasties were performed on 25 patients and only 7 benefited from an emergency aorto-coronary by-pass (all the patients who benefited from an emergency myocardial revascularization had preserved left ventricle ejection fractions).
Discharge status
By analyzing the patient’s condition at discharge we realized that approximately ¾ of the patients were discharged in a better state than the one they presented at admission, but the percentage of those discharged in a worse condition than the one they came in, or stationary, is not negligible (11.7% – were stationary from a clinical point of view, compared to their state at admission and 4.9% had an aggravated clinical status compared to the one they presented upon admission). The clinical examination performed at discharge revealed that almost half of the patients still presented signs of congestion: 16.27% – pulmonary congestion expressed through wet rales, 11.1% – peripheral congestion expressed through calf edema and 22% presented both signs.
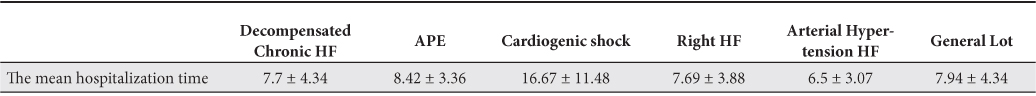
The mean hospitalization time in the general lot was 7.94±4.34 days, with statistically significant variations depending on the clinical forms of the disease. Cardiogenic shock, the most severe form of acute HF, registered the longest mean hospitalization time, whereas acute HF manifested during a hypertension peak registered the lowest values (Table 4).
Table 4. The mean hospitalization time (days) according to the clinical form of presentation
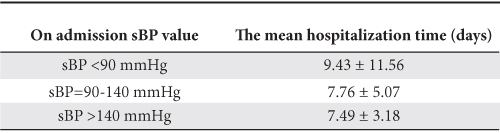
By analyzing the mean hospitalization period considering sBP values present at admission, we noticed that patients with arterial hypotension at admission (frequently due to cardiogenic shock) had the longest mean hospitalization time (Table 5).
Table 5. The mean hospitalization time according to the on admission sBP values (data from the general lot)
Mortality in the general lot was 10.61%, without any statistically significant differences between the study lots: 10.34% in the Galaţi lot, and 10.85% in the Bucharest lot. By analyzing mortality rates considering the 5 clinical forms of presentation, we discovered very high mortality rates in the cardiogenic shock group (86.4%). The acute pulmonary edema group and the one with acute right HF also registered high mortality rates, 13.2%, respectively 13.3%. None of the patients suffering from acute hypertensive HF died. Acute de novo HF registered high mortality rates (13.92%), compared to decompensated chronic HF (9.85%). The differences were statistically significant (p<0.05), but acute de novo HF did not prove to be an independent negative prognostic factor in the studied groups (p=0.14).
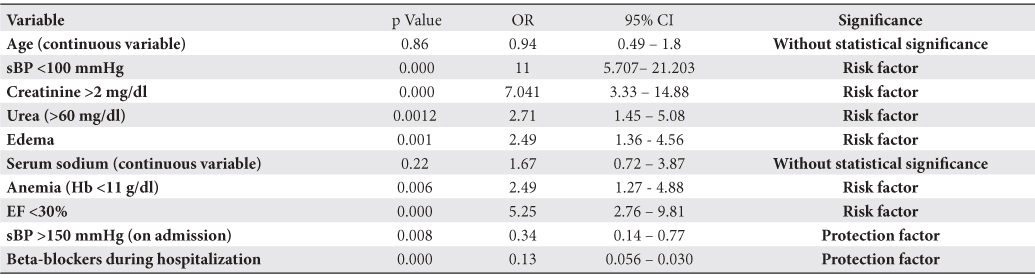
Prognostic factors
Several category and continuous variables were analyzed in order to identify negative prognostic factors during admission in the hospital: age, sex, values of systolic and diastolic blood pressure on admission, serum urea, serum creatinine, blood glucose, hemoglobin, serum sodium, peripheral edema, stasis rales present on admission, atrial fibrillation, diabetes, QRS duration >120 msec, tachycardia >100 bpm, ischemic etiology and medication during admission. By using a multivariate regression logistic model, we identified the following independent negative prognostic factors: arterial hypotension, renal dysfunction, peripheral edema, anemia and severe left ventricle systolic dysfunction. In contrast, high sBP on admission and the use of beta-blockers during the hospitalization were protection factors, associated with a positive prognostic. sBP, urea, creatinine, serum hemoglobin and the on-admission ejection fraction were analyzed as continuous variables. sBP became an independent negative prognostic factor for values lesser than 100 mmHg. In accordance with previous record, renal dysfunction was a negative prognostic factor in the study lots. Serum creatinine >2 mg/dl and serum urea >60 mg/dl at the time of presentation were independent negative prognostic factors. Severe left ventricle systolic dysfunction, defined for values of the ejection fraction lower than 30%, was an independent negative prognostic factor in the general lot. We noticed that hemoglobin <11 g/dl was an independent risk factor, associated with increased mortality rates. Peripheral edema, the clinical expression of peripheral congestion, represented a risk factor in the univariate analysis (Table 6).
Table 6. Prognostic factors in the general lot
Discussions
The results obtained from this study were compared to the results of the main acute HF registries developed up to the present time: ADHERE (Acute Decompensated Heart Failure National Registry), EHFS II (European Heart Failure Survey), EFICA (Etude Française de l’Insuffisance Cardiaque Aigue), Italian Survey (The Italian Registry of Acute HF), RRICA (The Romanian Registry of Acute Heart Failure) and ESC-HF Pilot – The Heart Failure Pilot Survey – European Society of Cardiology (ESC-HF Pilot)2-10.
Although this study enrolled patients from two different medical centers, with different investigation and treatment capacities, the differences in mortality rates are not significant. The mortality rate in the general lot (10.61%) is higher than the reported by RRICA (7.7%), but comparable to the data reported by the two cardiology units in the National Registry of Acute HF. Thus, the cardiology unit from Galaţi reported to RRICA a mortality rate of 10.6% and the cardiology unit from the academic hospital reported a rate of 11.4%8.
Mortality during hospitalization was 6.7% in EHFS II5. Mortality rates during hospitalization were significantly lower in ESC-HF Pilot compared to the other registries (only 71 patients). A predictive model for mortality could not be created due to the low number of deaths in this registry. Three independent variables were highlighted, all associated with increased mortality rates: sBP <110 mmHg, age >75 years and the deterioration of the renal function, expressed through the creatinine clearance rate <50 ml/min/1.73 m² 10.
Cardiogenic shock is the clinical form with the highest mortality rates, both in our lot, as well as in the literature. Mortality in cardiogenic shock was as high as 39.6% in EHFS II and 62.4% in RRICA5,8.
ADHERE was the first registry which promoted the concept of risk stratification in acute HF. Later, all the registries tried to reveal risk factors and protection factors during hospitalization, as well as after discharge. The CART-ADHERE model identified the following negative prognostic risk factors: sBP <115 mmHg, urea >43 mg/dl and creatinine levels >2.75 mg/dl. The large number of patients enrolled in this registry allowed its authors to create a predictive model by analyzing large number of variables (clinical and biological parameters, medical history data, etc.)2-4. EHFS II was the second large registry which promoted the concept of risk stratification in acute HF syndrome. This registry succeeded in identifying a series of prognostic factors regarding mortality rates at 3 months and one year. The negative prognostic factors were: age >75 years, history of myocardial infarction, renal dysfunction present on admittance, low sodium values (Na <135 mmol/l), anemia (Hb <12 g/dl), diabetes, left ventricle systolic dysfunction (EF <30%) and BMI <25 Kg/m². Only the values of the sBP at admission >160 mmHg was a favorable prognostic factor5. In the Italian Survey, another registry which identified prognostic factors, high sBP on admittance and a history of myocardial revascularization determined a better evolution for these patients. In opposition, the use of inotropic agents, high troponin level on admission, old age and renal dysfunction determined higher mortality rates7. In RRICA the factors associated with increased mortality rates during hospitalization were: the use of inotropic agents, the presence of ventricular arrhythmias during hospitalization, high serum urea values and age. The use of beta-blockers and high sBP represented protection factors in this registry8,9.
An important predictor for the negative evolution of patients suffering from both acute and chronic HF, hyponatremia did not influence mortality rates in a statistically significant manner in the study lots. Hyponatremia, traditionally defined as serum sodium values lower than 135 mmol/l loses its prognostic value in hyperglycemic patients. This statement is supported by a study performed on approximately 300 patients admitted for acute HF in a hospital from Tel Aviv11. We believe that the high percentage of patients with hyperglycemia at admission (especially in the lot from the non-academic hospital) can explain why hyponatremia was not a risk factor in this study.
High BP on admission (BP >150 mmHg) and the use of beta-blockers during admission were protection factors in the studied lots. These two variables were also considered protection factors in RRICA8,9. Otherwise, high sBP on admission was established to be a protection factor in most acute HF registries, both American (ADHERE), as well as European (Italian Survey, EHFS II)2-5,10. Surprisingly, age (especially >75 years) was not a risk factor which influenced mortality rates in a statistically significant manner. Most registries, including RRICA, Italian Survey and ESC – HF Pilot concluded, however, that age >75 years is a risk factor during hospitalization8-10. Low sBP and renal dysfunction on admission also proved to be negative prognostic factors in EFICA12. In the predictive models created after numerous studies, the ejection fraction was an inconstant presence among negative prognostic factors.
CONCLUSIONS
In the studied cohort, independent negative prognostic factors were: sBP on admission <100 mmHg, renal dysfunction (urea >60 mg/dl, creatinine >2 mg/dl), severe left ventricle systolic dysfunction (EF <30%), anemia (Hb <11 g/dl) and peripheral edema. From the variables which were statistically analyzed, sBP on admission >150 mmHg and the use of beta-blockers during admission were favorable prognostic factors. The negative prognostic factors identified in this study reflect the demographical, clinical and treatment particularities of patients with acute HF from this geographical area. These risk factors can also be found in the important acute HF registries, with variation from one geographical area to another. Mortality rates for patients hospitalized for acute HF remain high. In order to lower mortality rates for these patients, the treatment should be recommended taking into consideration these risk factors. For example, the concept of risk stratification, intensely promoted by the majority of registries for acute HF conducted up to the present time, brought great benefits for patients suffering from acute coronary syndromes. Due to the complexity and heterogeneity of acute HF syndrome, combined with the significant regional and national differences, the need for registries that include prospective, unselected patients became increasingly higher. These registries have the role of highlighting negative evolution prognostic factors, capable of organizing the patients into risk groups and receiving treatment in accordance with this classification.
Study limitations
We consider that this study has the following limitations: a relatively small number of patients, short enrollment period and a small number of medical centers involved.
Conflict of interests: none declared.
Bibliography
1. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008”– European Heart Journal 2008; 29:2388 – 2442
2. Yancy CV, Lopatin M, Stevenson LW, et al.”Clincal presentation, management and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the Acute Decompensated Heart Failure National Registry (ADHERE) database. Am Coll Cardiol 2006;47:76-84
3. Gheorghiade M, Filippatos Gerasimos. Reassessing treatment of acute heart failure syndromes: the ADHERE Registry. Eur Heart J supl.2005.B13-B19
4. ADHERE Scientific Advisory Committee: Acute Decompensated Heart Failure National Registry (ADHERE) Core Module Q1 2006 Final Cumulative National Benchmark Report: Scios, Inc,july 2006
5. Nieminen MS, Brutsaert D, Dickstein D, et al. Euroheart Failure Survey II (EHFS-II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J 2006, 27:2725-2736
6. Zannad F, Mebazaa A, Juilliere Y, et al: Clinical profile, contemporary management and one-year mortality in patients with severe acute heart failure syndromes: the EFICA study. Eur J Heart Fail 2006;8: 697-705
7. Tavazzi L, Maggioni AP, Lucci D, et al. Nationwide survey on acute heart failue in cardiology ward services in Italy. Eur Heart J 2006;27: 1207-1215
8. O. Chioncel – Registrul Român de Insuficienţă Cardiacă Acută (RRICA) – Congresul Naţional al Societăţii Române de Cardiologie, Sinaia 2010.
9. O. Chioncel, C. Macarie, M. Gheorghiade et al. The Romanian Acute Heart Failure Syndromes (RO-AHFS) Registry. American Heart Journal, feb. 2011
10. Aldo P. Maggioni, Ovidiu Chioncel, Gerassimos Filippatos et al. The Heart Failure Pilot Survey (ESC – HF Pilot). Eur J Heart Fail 2010. 12;
1076 – 1084
11. Olga Milo – Cotter, Gad Cotter, Beth D. Weatherley et al. Hyponatraemia in acute heart failure is a marker of increased mortality but not when associated with hyperglicaemia, Eur J Heart Fail; 10 (2008) 196-200
12. Chris Adamopoulus, Faiez Zannad, Renaud Fay et al. Ejection fraction and blood pressure are important and interactive predictors of 4-week mortality in severe acute heart failure. Eur J Heart Fail 2007, 4: 935-941
 This work is licensed under a
This work is licensed under a