Alina Hohaci1, Liviu Macovei1, Mircea Balasanian1,2, Lucian Stoica2,4, Nicusor Lovin3, Carmen Elena Plesoianu1,2, Larisa Anghel1,2, Ana Tanasa1, Maria Cristina Vladeanu1, Catalina Arsenescu Georgescu1,2
1 Discipline of Cardiology, “Prof. Dr. George I. M. Georgescu” Institute of Cardiovascular Diseases, Iasi, Romania
2 “Grigore T. Popa” University of Medicine and Pharmacy, Iasi, Romania
3 Department of Interventional Cardiology, “Prof. Dr. George I. M. Georgescu” Institute of Cardiovascular Diseases, Iasi, Romania
4 Discipline of Cardiothoracic Surgery, “Prof. Dr. George I. M. Georgescu”, Institute of Cardiovascular Diseases, Iaşi, România
Abstract: Introduction – Takotsubo cardiomyopathy (TCM) is a cardiac condition that mimics the clinical presentation of acute coronary syndrome, but without any evidence of obstructive atherosclerotic coronary artery disease. The prognosis is usually good, with improvement of the left ventricular (LV) dysfunction within a few weeks. There are some possible complications that may occur in the acute phase. Case presentation – We report the case of a 77 years old female patient, who presented with intense chest pain, occurred in conditions of a major emotional stress, associated with pulmonary oedema and cardiogenic shock. Echocardiographic exam showed the presence of a major mitral regurgitation (MR) in addition to the severely impaired LV systolic function (estimated ejection fraction of 20-25%). The patient underwent emergent coronary angiography, revealing no signifi cant coronary arteries lesions, but instead an image of LV “apical ballooning” at ventriculography, suggestive for TCM. The patient evolution was slightly favourable, under supportive medical treatment, with full recovery of the LV function at 4 weeks follow-up, and mild MR. Conclusion – This case illustrates an unexpected evolution of a critical patient, with severe LV dysfunction and acute ischemic MR, that had instead a full recovery, typical for TCM, which raised major difficulties in terms of diagnosis and management, but with excellent outcome.
Keywords: Takotsubo cardiomyopathy, acute mitral regurgitation, pulmonary oedema, cardiogenic shock, echocardiography.
INTRODUCTION
Takotsubo cardiomyopathy (TCM), also called transient left ventricular (LV) apical ballooning or “broken heart syndrome,” is a cardiac condition that mimics the clinical presentation of acute coronary syndrome, but without any evidence of obstructive atherosclerotic coronary artery disease (CAD)1-3. The incidence of TCM is postulated in most studies between 1% to 2.2% of ACS and is higher in postmenopausal women3-7. Emotional or physical stress at onset is common, although a triggering event is not always present3,7-8. Proposed etiopathogenic mechanisms include: multivessel coronary artery spasm, impaired cardiac microvascular function, endogenous catecholamine induced myocardial stunning and microinfarction or possible direct catecholamine-mediated myocyte injury1-6,9. Although it is considered to be a benign condition, with generally favourable outcome, there are possible complications that may occur in the acute phase (up to 50% of patients develop complications)10. Heart failure is the most common among it, mainly due to the impaired LV systolic function. There are also mentioned life-threatening arrhythmias, sudden cardiac death, right ventricular involvement, thrombus formation, resulting in stroke or arterial embolism or rarely, ventricular rupture4,10-13. Up to 20–25% of patients with TCM may develop acute mitral regurgitation (MR) and/or left ventricular outfl ow tract (LVOT) obstruction, severe complications that can significantly worsen the clinical patient status, leading to cardiogenic shock and/or pulmonary oedema, with major impact on vital prognosis7.
CASE PRESENTATION
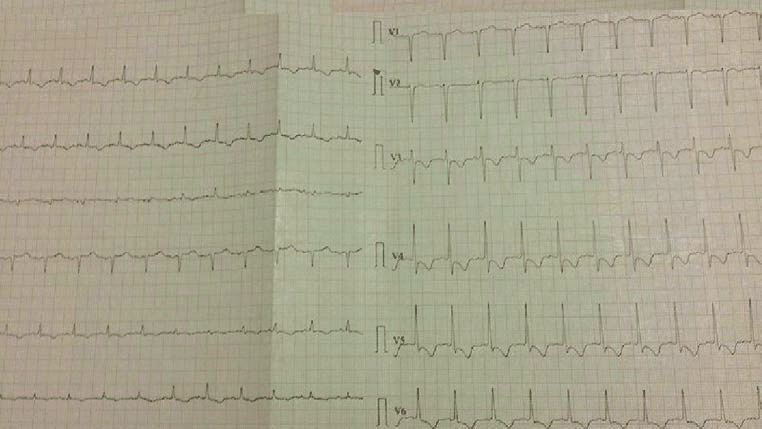
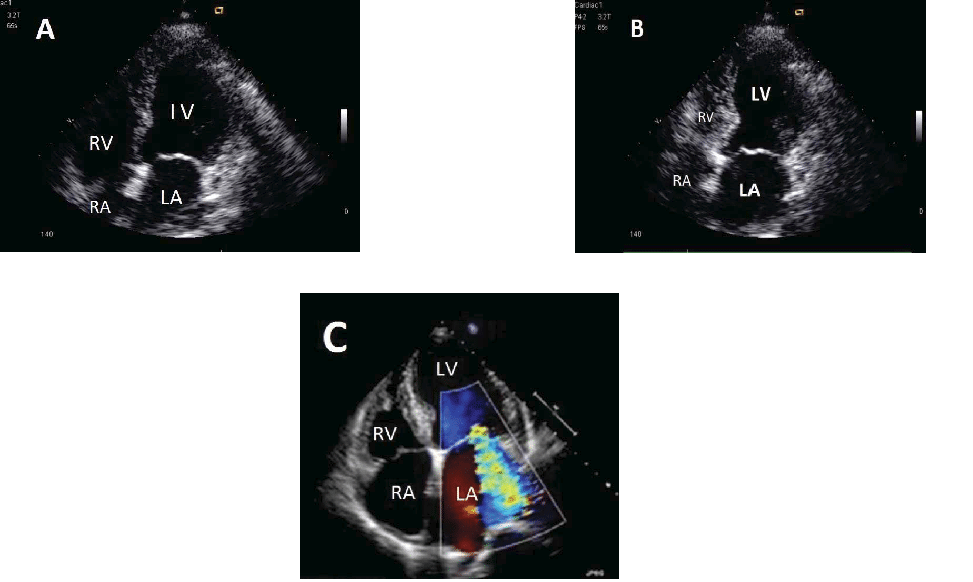
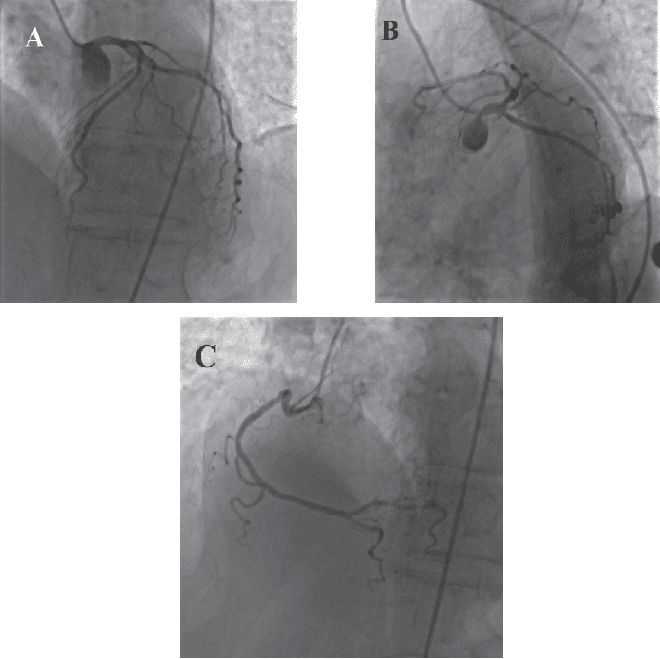
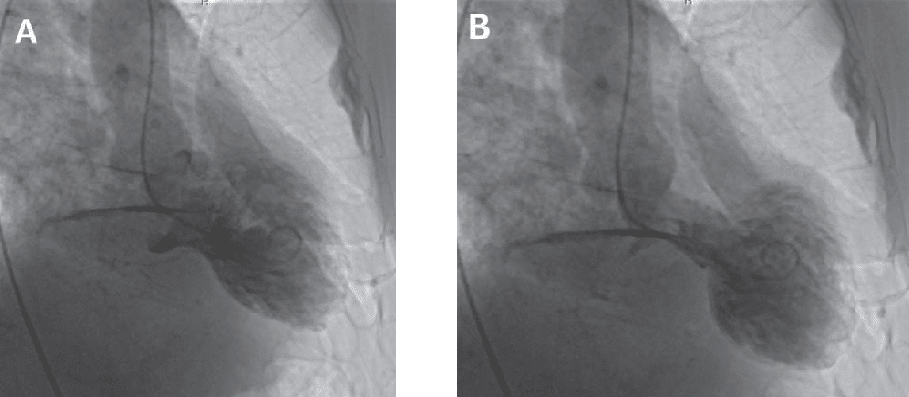
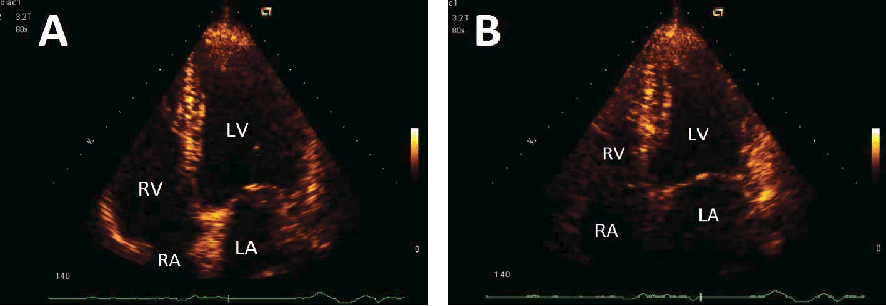
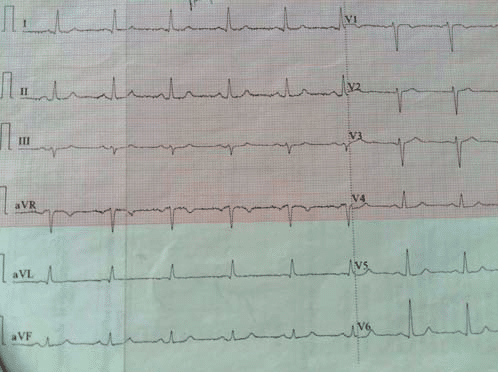
We present the case of a 77 years old female patient that was admitted in our emergency care unit at two hours after the onset of a persistent, intense, constrictive chest pain, associated with shortness of breath, occurred in conditions of a major emotional stress (unexpected loss of a son). She had never experienced a similar chest pain before. Her medical background included 20 years history of hypertension, treated intermittently with calcium channel blocker and type 2 diabetes mellitus, diagnosed 5 years ago, with inadequate glycemic control under treatment with Metformin. She had neither history of smoking nor family history of CAD. On presentation, the physical exam revealed a hemodynamic unstable patient, blood pressure (BP) of 80/50 mmHg, pulse of 100 beats/min, 90% oxygen saturation under the use of a face mask at 6 L/min, respiratory frequency of 30 breaths/min, chest pain present 6/10. Cardiac exam showed tachyrhythmic heart sounds, intense systolic murmur 3/6 at the apex, normal symmetrical peripheral pulse, inspiratory crackles over posterior bases in both lungs. The electrocardiogram (ECG) on admission showed sinus rhythm, ST segment depression followed by deep T-wave inversions in both anterior and inferior leads (Figure 1). The transthoracic echocardiography showed severe impaired LV systolic function (estimated ejection fraction- EF of 20-25%), with severe hypokinesia of the apex and the mid-apical segments of the LV walls and also severe mitral regurgitation (MR), with eccentrically directed posterior jet, normal-sized atrial cavities, no pericardial effusion (Figure 2). Laboratory exams showed elevated cardiac Troponin I (4 ng/ml, normal 0.0-0.3 ng/ml) with slightly elevated creatine kinase on admission (30 U/L, then normal values), normal lactate dehydrogenase and aspartate transaminase values, both on admission and in evolution, elevated pro-brain natriuretic peptide (1500 pg/ ml, normal 125 pg/ml), mild leucocytosis (12.000/mm3), elevated C- reactive protein (15 mg/L, normal 5 mg/L), normal creatinine levels, persistently elevated blood glucose levels (160 mg%-130 mg%) and dyslipidemia (total cholesterol 235 mg%, HDLc 40 mg%, LDLc 160 mg%, triglyceride 175 mg%). The patient underwent a coronary angiography, which showed no significant coronary artery lesions (Figure 3). Left ventriculography revealed severe hypokinesia of the apex, outlining an image of LV “apical ballooning”, suggestive for TCM (Figure 4). Under supportive medical treatment, with intravenous dobutamine and noradrenaline, the hemodynamic patient’s status improved. After reaching normal BP values, low doses of nitrates was used in order to relief dyspnoea. Furthermore, the evolution was slightly favourable, with symptoms relief and without arrhythmic events until discharge. Regarding the presence of acute significant MR, which was thought to be in the context of ischemia, according to the initial cardiovascular surgical evaluation, the mitral valve repair procedure was delayed, taking into account the severe LV systolic dysfunction. Treatment at discharged included antiplatelet therapy (acetyl salicylic acid), statine, beta-blocker and angiotensin-enzyme converting inhibitor in low doses (limitation for BP). At 4 weeks follow-up, at transthoracic echocardiographic examination it was noticed a full recovery of LV function and mild MR (Figure 5), aspects that further sustained the diagnosis of TCM. The patient was asymptomatic, without residual chest pain and the ECG showed normal morphology of QRS complex, without ST- T segment changes (Figure 6).
Figure 1. ECG on admission: sinus rhythm, 100 bpm, ST oblique descendent segment depression of 1- 2 mm in V3- V6 and deep T-wave inversions in DI, aVL, DII, aVF, V3- V6.
Figure 2. Transthoracic echocardiography on admission: end-diastolic (A) and end-systolic (B) apical four chamber view illustrating the typical apical and mid-ventricular LV ”ballooning” and severe MR associated (C).
DISCUSSIONS
This case illustrates a particular evolution of TCM, complicated by acute MR, pulmonary oedema and cardiogenic shock, which raised major issues in terms of management, considering the paucity of the literature data in this condition. There are several hypotheses regarding the mechanisms of acute MR associated with TCM. De Backer et al. showed in a two-year, two-center experience study, that up to 20% of TCM patients may develop left ventricular outfl ow tract (LVOT) obstruction, being in accord with some previous studies14-15. Factors associated with this complication were advanced age, septal bulging, systolic anterior motion (SAM) – induced MR, and hemodynamic instability7. In this study, all patients with LVOT obstruction developed SAM of the anterior mitral valve leaflet and high-grade MR, and nearly half of them presented cardiogenic shock7. On the other hand, Izumo et al. found in their study another mechanism involved: mitral valve leaflet tethering secondary to papillary muscle dysfunction or displacement associated with regional or global LV systolic dysfunction and LV enlargement16. This is previously known as an important cause of ischemic MR17-19. The transient ischemia, with classic LV apical “ballooning” and consecutively impaired LV systolic function is a common finding in TCM, those it is reasonable to be aware of the occurrence of acute MR in these conditions. In the case presented, echocardiography revealed besides a severely impaired LV systolic function, a major MR, but no signs of SAM or obstruction in LVOT. In the absence of SAM or LVOT obstruction, the low EF of 20-25%, together with the mid-apical ischemia and the LV apical ballooning, consists in arguments for the hypothesis of transient ischemic MR. Furthermore, the identifi cation of the specific mechanism of acute MR in this condition is important for proper management of the patients. For instance, in cases with LVOT obstruction associated, the use of inotropic agents or vasodilators, otherwise often used in the treatment of ACS, can worsen the grade of obstruction. Instead, there are recommended beta- blockers, fl uid intake or intra-aortic balloon pump (IABP), for refractory cardiogenic shock, as a bridge to clinical recovery4,7,20-21. In cases with MR without SAM, because of severe LV dysfunction associated, the inotrope therapy is often necessary, with the recommendation for careful titration of these in order to avoid triggering LVOT obstruction22-23. We used double association of inotrope agents, both dobutamine and noradrenaline, in order to obtain hemodynamic stability of our patient. Another important and disputed question was what is best to do regarding the indication of mitral valve replacement in these cases? The current European and American guidelines recommend mitral valve surgery in symptomatic patients with severe acute MR24-25. On the other hand, the fact that both LV dysfunction and MR associated with TCM are reversible, the idea of supportive medical treatment until complete recovery is feasible21,26. In the case presented, we asked for cardiovascular surgical evaluation, that suggested us to postpone the mitral valve replacement intervention, considering the
unacceptable high risk associated with the severe LV systolic dysfunction. The fact that we adopted a conservative strategy was the best thing to do in this case, which was confirmed later, when the patient returned after 4 weeks, with complete recovery of LV function and mild MR, that eliminated the previous indication of surgery.
Figure 3. Coronarography: left coronary artery (A. left anterior oblique cranial view; B. left anterior oblique caudal view) and right coronary artery (C. left anterior oblique view), both without significant lesions.
Figure 4. Ventriculography: LV end-diastolic (A) and LV end-systolic (B) view outlining the aspect of LV “apical ballooning”.
Figure 5. Transthoracic echocardiography after 4 weeks: end-diastolic (A) and end-systolic (B) apical four chamber view demonstrating the full recovery of LV systolic function, without wall motion abnormalities.
Figure 6. ECG after 4 weeks: sinus rhythm, 70 bpm, normal QRS morphology without ST-T changes.
CONCLUSIONS
Despite the mechanism involved, the association of significant acute MR in a patient with TCM, increases the risk of adverse outcomes. This underline the importance of an accurate diagnosis, systematic and repeated echocardiographic evaluations of a patient diagnosed with TCM, in order to unmask as earlier as possible such complication27. This case exposed the difficulties of diagnosis and treatment of a critical patient, presented with severe LV dysfunction and acute MR, leading to pulmonary oedema and cardiogenic shock that had an excellent recovery under conservative treatment, typical for TCM.
Acknowledgements: none declared.
Funding: none declared.
Conflicts of interest: none declared.
References
1. Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008;155:408–417.
2. Sharkey SW, Windenburg DC, Lesser JR, Maron MS, Hauser RG, Lesser JN, Haas TS, Hodges JS, Maron BJ. Natural history and expansive clinical profile of stress (tako-tsubo) cardiomyopathy. J Am Coll Cardiol. 2010;55:333–341.
3. Gianni M, Dentali F, Grandi AM, Sumner G, Hiralal R, Lonn E. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J. 2006;27:1523–1529.
4. Ghinghină C. Unclassifi ed cardiomyopathies. In Textbook of cardiology. Editura Academiei Române, Bucureşti, 2010, 387-389.
5. Sy F, Basraon J, Zheng H, Singh M, Richina J, Ambrose JA. Frequency of Takotsubo cardiomyopathy in postmenopausal women presenting with an acute coronary syndrome. Am J Cardiol. 2013;112:479–482.
6. Macovei L, Coada G, Constantinescu V, Arsenescu-Georgescu C. Takotsubo cardiomyopathy. Revista Medico-chirurgicala a Societatii de Medici si Naturalisti din Iasi 2012, 116(1):139-144.
7. DeBacker O, Debonnaire P, Gevaert S, Missault L, Gheeraert P, Muyldermans L. Prevalence, associated factors and management implications of left ventricular outfl ow tract obstruction in takotsubo cardiomyopathy: A two-year, two-center experience. BMC Cardiovasc Disord. 2014; 14: 147.
8. Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, Cammann VL, Sarcon A, Geyer V, Neumann CA, Seifert B, Hellermann J, Schwyzer M, Eisenhardt K, Jenewein J, Franke
J, Katus HA, Burgdorf C, Schunkert H, Moeller C, Thiele H, Bauersachs J, Tschöpe C, Schultheiss HP, Laney CA, Rajan L, Michels G, Pfi ster R, Ukena C, Böhm M, Erbel R, Cuneo A, Kuck KH, Jacobshagen C, Hasenfuss G, Karakas M, Koenig W, Rottbauer W, Said SM, Braun- Dullaeus RC, Cuculi F, Banning A, Fischer TA, Vasankari T, Airaksinen KE, Fijalkowski M, Rynkiewicz A, Pawlak M, Opolski G, Dworakowski R, MacCarthy P, Kaiser C, Osswald S, Galiuto L, Crea F, Dichtl W, Franz WM, Empen K, Felix SB, Delmas C, Lairez O, Erne P, Bax JJ, Ford I, Ruschitzka F, Prasad A, Lüscher TF. Clinical features and outcomes of takotsubo cardiomyopathy. N Engl J Med. 2015; 373: 929–938.
9. Apetrei E. Takotsubo cardiomyopathy. In Clinical Cardiology. Editura medicală Callisto, Bucureşti, 2015, 839-848.
10. Bossone E, Lyon A, Citro R, Athanasiadis A, Meimoun P, Parodi G, Cimarelli S, Omerovic E, Ferrara F, Limongelli G, Cittadini A, Salerno- Uriarte JA, Perrone Filardi P, Schneider B, Sechtem U, Erbel R. Takotsubo cardiomyopathy: an integrated multi-imaging approach. Eur Heart J Cardiovasc Imaging (2014) 15 (4): 366-377.
11. Weihs V, Szücs D, Fellner B, Eber B, Weihs W, Lambert T, Metzler B, Titscher G, Hochmayer B, Dechant C, Eder V, Siostrzonek P, Leisch F, Pichler M, Pachinger O, Gaul G, Weber H, Podczeck-Schweighofer A, Nesser HJ, Huber K. Stress-induced cardiomyopathy (Tako-Tsubo syndrome) in Austria. Eur Heart J Acute Cardiovasc Care. 2013; 2:137–146.
12. Pant S, Deshmukh A, Mehta K, Badheka AO, Tuliani T, Patel NJ, Dabhadkar K, Prasad A, Paydak H. Burden of arrhythmias in patients with Takotsubo Cardiomyopathy (apical ballooning syndrome) Int J Cardiol. 2013;170:64–68.
13. Brinjikji W, El-Sayed AM, Salka S. In-hospital mortality among patients with takotsubo cardiomyopathy: a study of the National Inpatient Sample 2008 to 2009. Am Heart J. 2012;164:215–221.
14. Parodi G, Del Pace S, Salvadori C, Carabba N, Olivotto I, Gensini GF. Left ventricular apical ballooning syndrome as a novel cause of acute mitral regurgitation. J Am Coll Cardiol. 2007;50:647–649.
15. El Mahmoud R, Mansencal N, Pilliére R, Leyer F, Abbou N, Michaud P. Prevalence and characteristics of LV outfl ow tract obstruction in Tako-Tsubo syndrome. Am Heart J. 2008;156:543–548.
16. Izumo M, Nalawadi S, Shiota M, Das J, Dohad S, Kuwahara E, etal. Mechanisms of acute mitral regurgitation in patients with takotsubo cardiomyopathy: An echocardiographic study. Circ Cardiovasc Imaging. 2011; 4: 392–8.
17. Kwan J, Shiota T, Agler DA, Popović ZB, Qin JX, Gillinov MA, Stewart WJ, Cosgrove DM, McCarthy PM, Thomas JD. Geometric differences of the mitral apparatus between ischemic and dilated cardiomyopathy with significant mitral regurgitation: real-time three-dimensional echocardiography study. Circulation. 2003;107:1135–1140.
18. Marwick TH, Lancellotti P, Pierard L. Ischaemic mitral regurgitation: mechanisms and diagnosis.Heart. 2009;95:1711–1718.
19. Haghi D, Röhm S, Suselbeck T, Borggrefe M, Papavassiliu T. Incidence and clinical signifi cance of mitral regurgitation in Takotsubo cardiomyopathy. Clin Res Cardiol.2010
20. Weiner MM, Asher DI, Augoustides JG, Evans AS, Patel PA, Gutsche JT, Mookadam F, Ramakrishna H. Takotsubo Cardiomyopathy: A Clinical Update for the Cardiovascular Anesthesiologist. J Cardiothorac Vasc Anesth. 2017 Feb;31(1):334-344.
21. Yin Wu, WuQiang F, Chachula L, Costacurta G, Rohatgi R, Elmi F. Left ventricular outfl ow track obstruction and mitral valve regurgitation in a patient with takotsubo cardiomyopathy. J Community Hosp Intern Med Perspect. 2015; 5(6): 10.
22. Ono R, Falcao LM. Takotsubo cardiomyopathy systematic review: Pathophysiologic process, clinical presentation, and diagnostic approach to takotsubo cardiomyopathy. Int J Cardiol. 2016; 209: 196–205
23. Stiermaier T, Eitel C, Desch S, Fuernau G, Schuler G, Thiele H, Eitel I.Incidence, determinants and prognostic relevance of cardiogenic shock in patients with takotsubo cardiomyopathy. Eur Heart J Acute Cardiovasc Care. 2016 Oct;5(6):489-496.
24. Vahanian A, Alfi eri O, Andreotti F, Antunes M J, Barón-Esquivias G, Baumgartner H, Borger M A, Carrel T P, De Bonis M, Evangelista A, Falk V, Iung B, Lancellotti P, Pierard L, Price S, Schäfers H J, Schuler G, Stepinska J, Swedberg K, Takkenberg J, Von Oppell U O, Windecker S, Zamorano J L, Zembal M. Guidelines on the management of valvular heart disease (version 2012). The Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2012;33:2470-2473.
25. Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, O’Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM 3rd, Thomas JD; American College of Cardiology/American Heart
Association Task Force on Practice Guidelines. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63: e57-e185.
26. Chandrasegaram MD, Celermajer DS, Wilson MK. Apical ballooning syndrome complicated by acute severe mitral regurgitation with left ventricular outfl ow obstruction–case report. J Cardiothorac Surg. 2007 Feb 21;2:14.
27. Citro R, Lyon AR, Meimoun P, Omerovic E, Redfors B, Buck T, etal. Standard and advanced echocardiography in takotsubo (stress) cardiomyopathy: Clinical and prognostic implications. J Am Soc Echocardiogr. 2015; 28: 57–74.
 This work is licensed under a
This work is licensed under a