Cristina Vacarescu1, Lucian Petrescu1,2, Emilia Violeta Goanta1, Simina Crisan1,2, Cristian Mornos1,2, Mihai Andrei Lazar1, Oana Patru1, Dragos Cozma1,2
1 Institute of Cardiovascular Diseases, Timişoara, Romania
2 Department of Cardiology, “Victor Babes” University of Medicine and Pharmacy, Timişoara, Romania
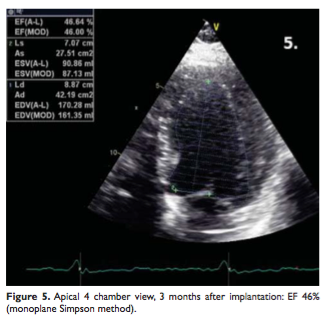
Abstract: Introduction – Several studies evaluated left ventricular only pacing in patients with classical CRT with similar outcomes compared to biventricular pacing, but few data exist about CRT using bicameral devices with only 2 leads right atrium/left ventricle (RA/LV). Case report – We present the case of a 42 y.o. male with idiopathic dilated cardiomyopathy, left bundle brunch block and symptoms of NYHA III class heart failure. Echocardiography showed severe global hypokinesia, EF 28 %, and mechanical dyssynchrony. With no evidence of ventricular arrhythmias and normal AV conduction, the patient had class I indication for CRT and was implanted with a bicameral pacemaker with only 2 leads RA/LV. At 3 months followup: echo examination showed important LV remodeling (EF 46%) and clinical improvement of NYHA class; same results were seen during the 5 years follow-up. This case report shows that bicameral pacemaker with only RA/LV leads may be considered an alternative to classic CRT in selected patients, as we showed in a recent small study1. We hoped that future large multicenter studies can better assess indications, efficiency and advantages for CRT using dual chamber RA/LV pacing.
Keywords: cardiac resynchronization therapy, synchronized left ventricular pacing, left ventricle only pacing.
Rezumat: Introducere – Stimularea unică de ventricul stâng a fost evaluată in câteva studii la pacienţii care au beneficiat de terapie de resincronizare cardiacă clasică (TRC) comparativ cu stimularea biventriculară, dar puţine date există despre TRC utilizând stimulatoare bicamerale cu doar 2 sonde la nivel atriu drept/ventricul stâng (AD/VS). Prezentare de caz – pacient, 42 de ani, diagnosticat cu cardiomiopatie dilatativa idiopatică, bloc major de ramură stângă şi simptome de insuficienţă cardiacă (IC) NYHA III. Ecocardiografic – hipokinezie globală severă, FE = 28%, parametrii de asincronism mecanic prezenţi. Având conducere atrioventriculară normală şi fără istoric de aritmii ventriculare, pacientul a beneficiat de TRC utilizând un stimulator bicameral cu 2 sonde la nivel AD/VS. La 3 luni post implant s-a constatat ecografic o remodelare importantă a VS (FE 46%) şi ameliorarea simptomelor de IC; aceleaşi rezultate s-au păstrat şi la 5 ani postimplant. Această prezentare susţine că resincronizarea bicamerală AD-VS poate reprezenta o alternativă la stimularea triplucamerală la pacienţii selectaţi, aşa cum am demostrat intr-un studiu publicat recent1. Sunt necesare studii multicentrice mari pentru a realiza o analiză a costurilor şi o evaluare complexă a acestei strategii.
Cuvinte cheie: terapie de resincronizare cardiacă, stimulare cu fuziune, stimulare unică de ventricul stâng.
INTRODUCTION
ESC guidelines on cardiac pacing and resynchronization therapy recommends LV only pacing in non-pacemaker dependent patients to decrease the cost and complexity of the procedure and increase the longevity of the device, particularly appealing in children and young adults.
In this report, we describe the case of a patient with idiopathic dilated cardiomyopathy associated with left bundle branch block and echocardiographic evidence of mechanical dyssynchrony but normal atrioventricular (AV) conduction, who met the criteria for CRT, in whom a bicameral pacemaker with 2 leads right atrium/left ventricle was implanted (RA-LV CRT). We also briefly review several studies in which safety and efficiency of LV pacing were analyzed in patients with biventricular pacing (BiV) by switching to LV only mode. To the best of our knowledge, this is the first case report regarding dual chamber RA-LV CRT.
CASE REPORT
A 42 years old male, smoker, hypertensive, was admitted to our clinic with symptoms of NYHA III class heart failure (HF). Physical examination revealed normal blood pressure 130/80 mmHg, III/VI systolic murmur in the mitral area, moist crackles halfway up bilaterally and lower extremity pitting edema. Laboratory tests showed normal renal and hepatic function but with impaired glucose tolerance. The electrocardiogram performed at admission showed sinus rhythm with a pattern of left bundle branch block and a QRS complex of 160 ms (Figure 1.a). The ECG Holter monitoring showed an average heart rate of 73 b/min, without evidence of ventricular arrhythmias.
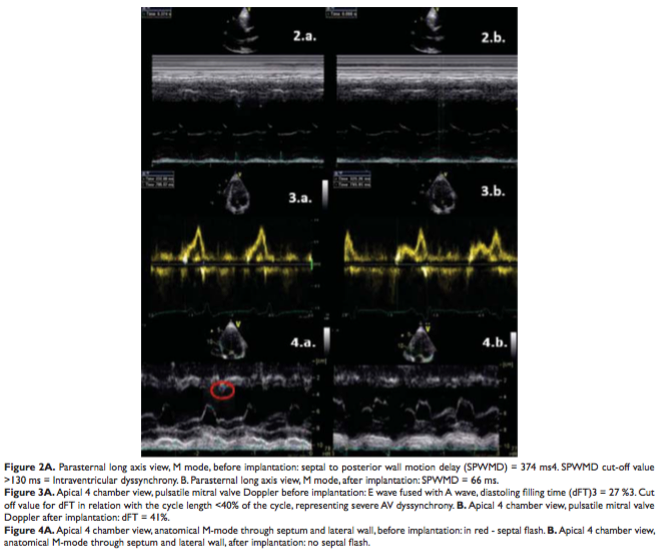
Transthoracic echocardiography revealed important LV dilatation: LV end diastolic diameter (LVEDD) 65 mm, end diastolic volume (EDV) 244 ml; severe global LV hypokinezia, ejection fraction (EF) 28 %; mild functional mitral regurgitation, moderate left atrium dilatation – 80 ml and type I diastolic dysfunction. Echocardiographic parameters of asynchrony were assessed with evidence of: intraventricular dyssynchrony (Figure 2.a) septal to posterior wall motion delay (SPWMD) 375 ms; atrioventricular dyssynchrony (Figure 3.a) duration of left ventricular filling in relation with the cycle lenght (dFT) 27%; septal flash in apical 4-chamber view (Figure 4.a).
Coronary angiography was performed and coronary artery disease was exluded.
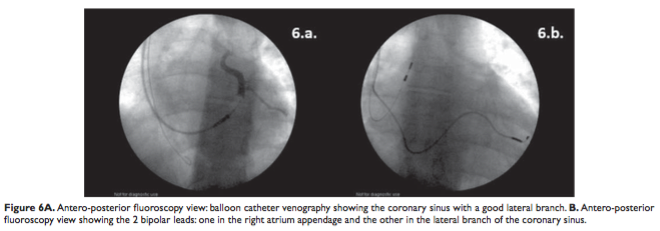
Bicameral RA/LV pacemaker was implanted using direct punction of left subclavian vein without incision, with following steps: 1. the LV lead was the first to be implanted after performing coronary sinus (CS) venogram using balloon catheter (Figure 6.a), a LV bipolar lead was placed into a lateral branch of the CS (Figure 6.b); 2. incision and fixation LV lead (consecutive subcutaneous pocket dissection); 3. bipolar RA lead (passive fixation/ appendage).
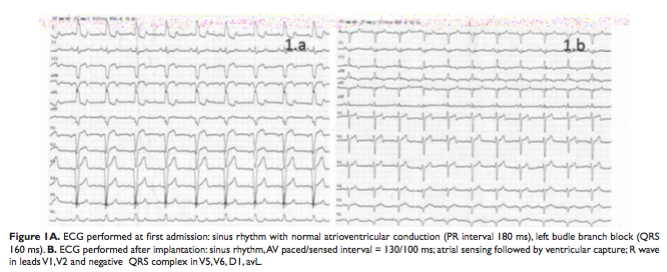
 The AV p/s interval was programmed at 130/100 ms in order to allow native RV depolarization and to preexcite LV. The ECG post implant (Figure 1.b) showed right axis deviation + 100 degree (from -30 degree), QRS complex 120 ms (from 160 ms), with rS pattern in V1.
The AV p/s interval was programmed at 130/100 ms in order to allow native RV depolarization and to preexcite LV. The ECG post implant (Figure 1.b) showed right axis deviation + 100 degree (from -30 degree), QRS complex 120 ms (from 160 ms), with rS pattern in V1.
In-hospital treatment with loop diuretic, aldosterone antagonist, ACE inhibitor and betablocker was continued after discharge. Heart rate management was easily obtained using only betablocker and complete ventricular capture close to 100% was achieved at discharge.
At 3 months follow-up the patient, although in NYHA functional class II, was hospitalized for reevaluation. The PM interrogation showed ventricular pacing 99%, without episodes of VT or SVT. Ventricular capture was also assessed by ECG Holter monitoring which excluded pseudofusion beats.
The echography revealed important revers remodeling of LV (Figure 5) with EDV 170 ml (from 244 ml) with increased EF 46% (from 28%), and improvement in atrioventricular and intraventricular asynchrony parameters (Figure 2.b, 3.b, 4.b). We performed exercise test (Bruce Protocol using cycle ergometer): the exercise time was 07:16 min, maximum exercise load was 160 Watts (6.7 METS), maxim heart rate 118 b/min (in treatment with betablocker), without loss of capture during the exercise. The patient was discharged maintaining the same PM programming and the same treatment.
The patient was evaluated at 6 months and yearly after, with a total follow-up period of 5 years since the CRT was performed. Ecocardiography, Holter ECG monitoring and exercise test were done at every admission in the hospital. The revers remodeling process of LV was maintained over time, at 5 year follow-up the patient had mild global hipokinesia, with EF 45% and EDV 156 ml, no worsening of mitral regurgitation and left atrium dilatation was noted since basal ecocardiography. Holter ECG monitoring showed ventricular paced rhythm 99%, without episodes of VT or SVT. The annual exercise tests performed revealed good exercise tolerance. Mean exercise time was 5.9 ± 2.7 min with an exercise load of 158 ± 14 Watts and a maximum heart rate of 119 ± 12 bpm (under betablocker). Loss of ventricular capture occurred in 2 of the exercise tests and was due to physiological shortening of the PR interval. The adaptive AV interval was shortened and several modulation rate parameters were changed, such as activity sensor threshold, slope and reaction time, and the exercise tests were repeated without loss of capture.
Pharmacological therapy readjustments were made during the 5 year follow-up. Oral antidiabetes treatment with glimepiride was introduced in the second year of follow-up since the patient developed type 2 diabetes mellitus. Treatment with loop diuretic, aldosterone antagonist, ACE inhibitor and betablocker was continued since baseline in stable doses.
DISCUSSIONS
Several studies assessed the efficiency of LV only pacing in CRT. BELIEVE study states that LV pacing is both safe and feasible, with a significant increase of EF at 12 months follow-up and a similar percentage of responders to LV only pacing as compared to BiV pacing5. B-LEFT HF trial also supports that LV only pacing is non inferior to BiV pacing regarding the clinical and echocardiographic response6.
The superiority of BiV pacing over LV pacing remains uncertain, but the rate still high of non-responders to classical CRT made reasonable LV only pacing as an alternative to BiV pacing in selected patients. GREATER-EARTH study is a multicenter, double-blind, cross-over trial in which 211 patients from 11 centers were randomized for LV only pacing followed by BiV pacing or vice-versa for consecutive 6 months periods. The study concluded that LV pacing is not superior to BiV pacing, but a respective 21% of patients who did not respond clinically and 17% of patients who did not respond ecocardiographycal to BiV pacing responded to LV pacing mode7.
Both clinical and experimental studies have shown that RV pacing leads to ventricular dyssynchrony with detrimental effects on cardiac structure and function. Recent DANPACE trail concluded that no association between the amount of RV pacing and clinical outcome was observed in patients with preserved EF, however the extent of the long-term clinical effects of RV pacing in patients with normal ventricular function are still scarce and subject to future investigation8,9. RV pacing worsens mechanical ventricular dyssynchrony in patients with low EF10,11. RV activation duration seems to be different in patients with HF during RV pacing, CRT with biventricular pacing or CRT using only LV only pacing. In patients with HF, normal RV free wall activation in intrinsic rhythm indicates normal right bundle brunch mediated depolarization; during RV pacing alone or with CRT-BiV, the LV was vulnerable to develop activation delays. LV only pacing can avoid perturbation of RV electrical perturbation12. In support of this idea, adapted CRT algorithm provides synchronized LV pacing to produce fusion with the intrinsic depolarization in patient with normal AV conduction. The adaptive CRT trial states that synchronized LV pacing has better clinical outcomes compared to echocardiographic optimized Biv pacing13.
Few data are available regarding CRT using bicameral devices with only 2 leads RA/LV.This option to classical CRT is understudied despite numerous potential advantages (less material, reduced procedural time, potential cost benefits). A recent small study1 on CRT using only RA/LV pacing in patients with idiopathic dilated cardiomyopathy showed a positive outcome and increased EF after an average follow up of 29.3±14.6 months. It is hoped that future multicenter studies can better assess indications, efficiency and advantages for dual chamber RA/LV pacing.
Conflict of interest: none declared.
References
1. D. Cozma, E.V. Goanta, C. Vacarescu, Mid-Term Follow Up In CRT Patients Using Only Right Atrium And Left Ventricular Leads With Fusion Pacing, Journal of Atrial Fibrillation, Octomber 2015
2. European Society of Cardiology (ESC), European Heart Rhythm Association (EHRA), Brignole M. 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: the task force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Europace 2013 Aug; 15:10701118.
3. Cazeau S, Bordachar P, Jauvert G, Lazarus A, Alonso C, Vandrell MC, Mugica J, Ritter P. Echocardiographic modeling of cardiac dyssynchrony before and during multisite stimulation: a prospective study. Pacing Clin Electrophysiol. 2003 Jan;26(1 Pt 2):137-43.
4. Pitzalis MV, Iacoviello M, Romito R, Massari F, Rizzon B, Luzzi G, Guida P, Andriani A, Mastropasqua F, Rizzon P. Cardiac resynchronization therapy tailored by echocardiographic evaluation of ventricular asynchrony. J Am Coll Cardiol. 2002;40(9):1615-22
5. Gasparini M, Bocchiardo M, Lunati M, Ravazzi PA, Santini M, Zardini M, Signorelli S, Passardi M, Klersy C. Comparison of 1-year effects of left ventricular and biventricular pacing in patients with heart failure who have ventricular arrhythmias and left bundle-branch block: the Bi vs Left Ventricular Pacing: an International Pilot Evaluation on Heart Failure Patiens with Ventricular Arrhythmias (BELIEVE) multicenter prospective randomized pilot study. Am Heart J. 2006 Jul; 152(1):155. e1-7.
6. Boriani G, Kraning W, Donal E, Calo L, Casella M, Delarche N, Lozano IF, Ansalone G, Biffi M, Boulogne E, Leclercq C. A randomized double blind comparison of biventricular versus left ventricular stimulation for cardiac resynchronization therapy: the Biventricular versus Left Univentricular Pacing with ICD back-up in Heart Failure Patients (BLEFT HF) trial. Am Heart J. 2010 Jun; 159(6):1052-1058.e1.
7. Thibault B, Harel F, Ducharme A, White M, Frasure-Smith N, Roy D, Phillippon F, Dorian P, Talajic M, Dubuc M, Gagne P, Guera PG, Macle L, Rivard L, Khairy P. Evaluation of cardiac resynchronization therapy for heart failure in patients with a QRS duration greater than 120 ms (GREATER-EARTH) trial. Circulation. 2011;124:2874-2881. Akerström F, Arias MA, Pachón M, Jiménez-López J, Puchol A, JuliáCalvo J. The importance of avoiding unnecessary right ventricular pacing in clinical practice. World J Cardiol. 2013 Nov 26;5(11):410-9. doi: 10.4330/wjc.v5.i11.410.
Akerström F, Pachón M, Puchol A, Jiménez-López J, Segovia D, Rodríguez-Padial L, Arias MA, Chronic right ventricular apical pacing: adverse effects and current therapeutic strategies to minimize them. Int J Cardiol. 2014 May 15;173(3):351-60. doi: 10.1016/j.ijcard.2014. 03.079. Epub 2014 Mar 20.
Schmidt M, Rittger H, Marschang H, Sinha AM, Daccarett M, Brachmann J, Block M, Breithardt OA. Left ventricular dyssynchrony from right ventricular pacing depends on intraventricular conduction pattern in intrinsic rhythm. Eur J Echocardiogr. 2009 Aug;10(6):776-83. doi: 10.1093/ejechocard/jep069. Epub 2009 Jun 10.
Schmidt M, Brömsen J, Herholz C, Adler K, Neff F, Kopf C, Block M Evidence of left ventricular dyssynchrony resulting from right ventricular pacing in patients with severely depressed left ventricular ejection fraction. Europace. 2007 Jan;9(1):34-40.
Varma N, Jia P, Ramanathan C, Rudy Y RV electrical activation in heart failure during right, left, and biventricular pacing, JACC Cardiovasc Imaging. 2010 Jun;3(6):567-75. doi: 10.1016/j.jcmg.2009.12.017. Birnie D, Lemke B, Aonuma K, Krum H, Lee KL, Gasparini M, Starling RC, Milasinovic G, Gorcsan J 3rd, Houmsse M, Abeyratne A, Sambelashvili A, Martin DO, Clinical outcomes with synchronized left ventricular pacing: analysis of the adaptive CRT trial. Heart Rhythm. 2013 Sep;10 (9):1368-74. doi: 10.1016/j.hrthm.2013.07.00.
 This work is licensed under a
This work is licensed under a