Mircea Balasanian¹,², Ovidiu Mitu¹,², Ana Nicolae², Catalina Arsenescu Georgescu¹,²
1 „Grigore T. Popa” University of Medicine and Pharmacy, Iaşi, Romania
2 „Prof. Dr. G.I.M. Georgescu” Institute of Cardiovascular Diseases, Iaşi, Romania
CASE PRESENTATIONS
We present the case of a 69-year old male patient, obese, dyslipidemic, former smoker (30 pack-years) who was admitted for shortness of breath and orthopnoea started two days before. His past medical history consisted of deep vein thrombosis in the left lower limb for approximately two months that was therapeutically neglected. Clinical examination revealed: sinus tachycardia 110 bpm, blood pressure 110/70 mmHg, respiratory rate 32/minute, oxygen saturation 88% at room air, no fever, and painful and swollen left lower limb.
Electrocardiogram at rest showed sinus rhythm 110 bpm, right bundle branch block, S1Q3T3 pattern and negative T waves in leads V1-V4. Laboratory exams: high-positive D-dimer; presence of inflammatory syndrome (leucocytes 14500/mm3, fibrinogen 641 mg/dl, CRP 61.4 mg/l); moderate elevated myocardial enzymes (cardiac troponine I 1.03 ng/ ml, CK-MB 28 U/L, LDH 522 U/L, AST 68 U/L); hypercholesterolemia (total cholesterol 226 mg/dl, LDL cholesterol 151 mg/dl); normal renal function, electrolytes and fasting glucose. Transthoracic echocardiography revealed acute right heart dilatation, medium right ventricle (RV) diastolic diameter 49 mm, RV lateral wall 4 mm, with RV compressing the left ventricle (LV), interventricular septum (IVS) with paradoxical movement, RV free wall hypokinesia, tricuspid annular plane systolic excursion (TAPSE) 15 mm, RV systolic pressure 39 mmHg (estimated systolic pulmonary arterial pressure – 60 mmHg) – all indirect aspects of high probability of pulmonary embolism (PE). Moreover, we could visualize serpiginous mobile thrombus located in the RA prolapsing in the RV with maximum length 54 mm (Figures 1, 2). Taking into consideration the high probability of PE and according to the latest guidelines1, Pulmonary Embolism Severity Index (PESI) of 139 points included the patient into the very high risk class. Considering the RV overload, the cardiovascular
surgeon contraindicated a surgical approach of the thrombus. Thus, based on surgeon opinion, clinical examination, laboratory exams, electrocardiographic and echocardiographic
aspects, we decided to perform systemic thrombolysis to the patient. We have chosen streptokinase with the following regime: 250 000 UI in bolus for 30 minutes, followed by 100 000 UI / hour for 36 hours. Afterwards, unfractionated heparin was continued until proper oral anticoagulation was obtained. Echocardiography reevaluation after 24-hour postthrombolysis showed the absence of intracavitary thrombus with RV function improvement, normal kinetic of IVS, RV systolic pressure reduced to 23 mmHg (estimated systolic pulmonary arterial pressure – 35 mmHg), TAPSE 20 mm (Figures 3, 4).

Figure 1. Subcostal view: serpiginous mobile thrombus (white arrow) prolapsed during diastole from right atrium (RA) into right ventricle (RV); black arrow indicates tricuspid annulus.

Figure 2. Subcostal view: same mobile thrombus (white arrow) located in RA during systole; black arrow indicates tricuspid valve. Figures 1 and 2 indicates the mobility of the thrombus during cardiac cycle.
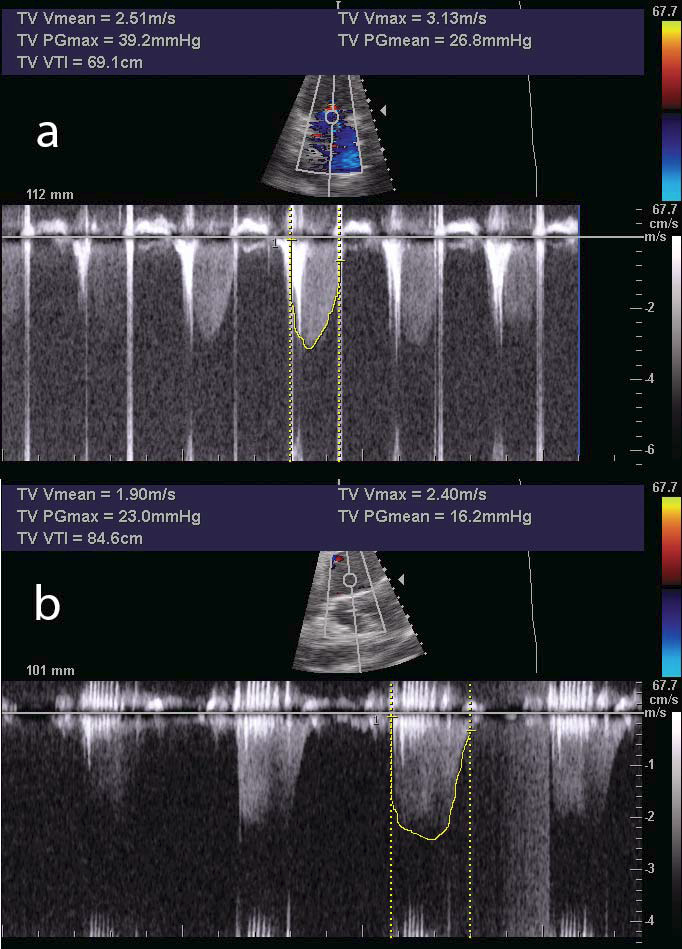
Figure 3. Tricuspid regurgitation continuous wave Doppler velocity before (a) and after (b) thrombolysis showing the acute reduction in right ventricular systolic pressure (from 39 to 23 mmHg).

Figure 4. Subcostal view: absence of thrombus after 24 hours of thrombolysis.
Pulmonary artery computer tomography revealed normal main pulmonary arteries with distal thrombus in the left pulmonary artery and non-occlusive thrombi in subsegmentary branches (Figure 5). The patient evolution was favorable during hospitalization, without hemodynamic impairment or postthrombolysis complications. After seven days, the patient was discharged with indication of oral anticoagulation for long term.
DISCUSSION
Mobile right heart thrombus represents a rare situation in the presence of acute PE, with a prevalence varying from 4 to 18%1. It is considered a major therapeutic emergency as it is associated with high rates of mortality (more than 20%) while in untreated patients the mortality is up to 90-100%2. Moreover, patients with right heart thrombi are more hemodynamically compromised by presenting acute early symptoms, congestive heart failure, lower blood pressure and important RV hypokinesis, with higher overall mortality
rates3. Anticoagulation with heparin, thrombolysis, surgical embolectomy and percutaneous catheter intervention are indicated as treatment in acute PE. However, the presence of free-fl oating right heart thrombi complicates the management and no specific recommendations are made for this particular setting. Recently, Athappan et al. showed on a pooled analysis over 320 patients which compared all up-mentioned methods of treatment that the lowest mortality was obtained in patients with thrombolysis and surgical embolectomy
compared to heparin anticoagulation only (13.7%, 18.3% and 37.1%, respectively). After multivariate analysis, the best survival rate in hemodynamically unstable patients was seen in thrombolysed patients compared to surgery or anticoagulation (81.5%, 70.4% and 47.7%, respectively) with no signifi cantly increased risk of hemorrhagic complications4. Another retrospective study revealed the lowest mortality rates for thrombolysis in comparison with surgical embolectomy, anticoagulation therapy or no therapy (11.3%, 23.8%, 28.6% and 100%, respectively)2. In our case, the thrombolytic treatment was the first line option and no thrombi were observed after 24 hours of treatment. Thrombolysis represents a
simple and effective method with various advantages including fast reduction of the pulmonary artery pressure and improvement of RV function by dissolving the intracardiac or pulmonary thrombi5. However, especially in patients with mobile right heart thrombi, the risk of clot detachment and further embolization to the lungs which are already affected is even higher. Another study that evaluated the thrombolytic treatment in PE showed that out of 12 patients with right heart thrombi, three died before the onset of treatment,
seven had a good evolution while two subjects had to perform adjunctive surgery because the persistence of massive thrombus6. Thus, surgical embolectomy represents another treatment option and is indicated especially in hemodynamically unstable patients where thrombolysis is contraindicated or ineffective. However, more evidence suggest that this procedure is associated with low mortality when early performed and may be extended to hemodynamically stable patients with RV dysfunction7. Pulmonary hypertension (PH) is another positive element for PE, with good prognosis both for the diagnosis and chronic thromboembolic pulmonary hypertension. In our case, the acute PH was moderate (55 – 60 mmHg) and after thrombolysis the value reduced to 35 mmHg. This may be explained by the rapid and effi cient onset of thrombolytic treatment which has been proven to better reduce the acute PH compared to patients that did not receive thrombolysis8. Moreover, the presence of RA thrombus might be another contributor to the increased PH at presentation.
CONCLUSIONS
Acute pulmonary thromboembolism represents one of the major cardiovascular emergencies by having a vital risk especially if it is associated with mobile right heart thrombus. Heparin anticoagulation, percutaneous catheter intervention, thrombolysis or surgical embolectomy are the treatment of choice, with better results for the last two options. No certain guideline recommendations are made for this particular situation and the treatment should be conducted by guiding after local possibilities and experience. Further studies
should be performed in order to establish which method is more effi cient and with lower risk.
Conflict of interest: none declared.
References
1. Konstantinides SV, Torbicki A, Agnelli G et al. 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J 2014; 35(43): 3033-69.
2. Rose PS, Punjabi NM, Pearse DB. Treatment of right heart thromboemboli. Chest 2002; 121(3): 806-14.
3. Torbicki A, Galié N, Covezzoli A, Rossi E, De Rosa M, Goldhaber SZ. Right heart thrombi in pulmonary embolism: results from the International Cooperative Pulmonary Embolism Registry. J Am Coll Cardiol 2003; 41(12): 2245-51.
4. Athappan G, Sengodan P, Chacko P, Gandhi S. Comparative efficacy of different modalities for treatment of right heart thrombi in transit: a pooled analysis. Vasc Med 2015; 20(2): 131-8.
5. Nkoke C, Faucher O, Camus L, Flork L. Free Floating Right Heart Thrombus Associated with Acute Pulmonary Embolism: An Unsettled Therapeutic Diffi culty. Case Rep Cardiol 2015, doi: 10.1155/2015/ 364780.
6. Pierre-Justin G, Pierard LA. Management of mobile right heart thrombi: a prospective series. Int J Cardiol 2005; 99(3): 381-8. 7. Samoukovic G, Malas T, deVarennes B. The role of pulmonary embolectomy in the treatment of acute pulmonary embolism: a literature review from 1968 to 2008. Interact Cardiovasc Thorac Surg 2010; 11(3): 265-70.
8. Casazza F, Bongarzoni A, Forgione C, Cuccia C, Imperadore F, Arrigo G, Floriani I, Pignataro L. Echocardiographic evolution of pulmonary artery pressure after acute pulmonary embolism. Results from IPER registry. Thromb Res 2014; 134(6): 1224-8.
 This work is licensed under a
This work is licensed under a