Sergiu Sipos1, Radu Ciudin1, Carmen Ginghina1
1 University of Medicine and Pharmacy “Carol Davila” Bucharest, Emergency Institute for Cardiovascular Diseases “Prof. Dr. C.C. Iliescu”, Bucharest
INTRODUCTION
It’s been over 50 years since the fi rst pacemakers were invented. Since then, important changes have been introduced concerning bradycardias, but also anti-tachycardia therapies such as anti-tachycardia pacing, internal defi brillation and devices aimed to improve synchronization in the failing heart. There is a dynamic regarding the indications for these therapies, which was imposed by the technical development of these incredible “mini”-computers, a process that still goes on today. Historically, there were experiments regarding cardiac resynchronization (CRT) starting with 1986 (Burkhoff et al) and also in 1990 (Latucca et al), by using animal models. Eight years later (1994) the first CRT was surgically implanted in a human being – Serge Cazeau. In 1998 Daubert (et al) presented the technique using the coronary sinus and later in 2001 FDA approved the use of this new therapy in humans (US). Very important, in the same year (2001) we had the fi rst CRT-P device implanted in our country and in 2003 the fi rst CRT-D implanted in Bucharest and Timisoara. Interesting is that the theoretical foundation for CRT was understood years after the fi rst implants, only when the modern imaging of the depolarization fronts, which occur in a dyssynchronized heart, was available. The principle of CRT consists in left and right ventricular pacing (bi-ventricular pacing) synchronized with the atrial (spontaneous or paced) activity. The pulse generator can be a three chamber pacemaker with or without defi brillator function. Thus, by optimizing cardiac electrical intervals, one can hope in the end to improve the cardiac output1,3,14.
SUBSTRATE OF HEART FAILURE – CARDIAC DYSSYNCHRONIZATION
The foundation of CRT lies in electrical and mechanical heart dyssynchronization which occurs in over a quarter of all the heart failure patient population. This form of heart failure is now regarded as a separate entity of chronic cardiac insuffi ciency. The presence of electrical heart dyssynchrony is responsible of immediate and important contraction impairment, as it is known from studies regarding right ventricular (RV) pacing (induced left bundle branch block (LBBB)). The electrical activating sequence in LBBB describes a U-shape pattern, “turning around the apex”: septum – apex – inferior wall – lateral wall, because of a functional blocking line which is orientated from LV base to the apex. Local contraction becomes time-variable, which leads to local strain impairment. Furthermore, these abnormalities cause regional myocardial differences in terms of work load. The last regions to depolarize have to deal with the highest work load. Globally, the entire heart suffers from pump defi ciency4. There are three levels of mechanical asynchrony: the first level is atrial-ventricular – it is responsible for reducing the diastolic fi lling time and the initiation of diastolic mitral regurgitation; the second one is the inter-ventricular asynchrony – it represents early activation of the RV with direct consequences over the interventricular septum contraction, which causes a decrease in LV performance; the third and most important is the intra-ventricular asynchrony – it is the result of early activation of the septum and late activation of the lateral wall as presented before (some authors consider the interventricular form as part of the intra-ventricular asynchrony)2,4,14.
INDICATIONS FOR THE CRT
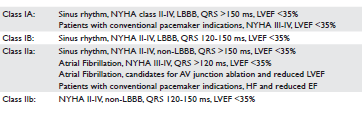
CRT represents one of the most modern and useful treatment techniques aimed to alleviate heart sufferance. The early conducted studies, at the beginning of the CRT era (about two decades ago), were small-size medical investigations which rapidly showed improvement in systolic LV function and cardiac output. From that point on, as the experience regarding implants grew and the number of CRT treated patients expanded considerably, large scale studies were possible and our understanding of this phenomenon gradually increased. The fi rst important changes concerning indication for CRT came with the 2012 ACCF/AHA/HRS Focused Update for CRT, where clear specifi cations in respect of NYHA Class severity, QRS morphology and duration, presence of sinus rhythm or atrial fi brillation, were made30. The early CRT studies focused only on QRS duration and the severity of heart failure5. Later, the high understanding of the relationship between symptom improvement and the decrease in cardiac dyssynchronism lead to further investigation of the potential effects of multisite biventricular pacing and intraventricular conduction delay (MUSTIC trial). This trial proved important symptomatic benefi ts in CRT patients, especially among class III NYHA, EF <35% and QRS duration over 150 ms6. QRS duration was also largely debated in the 2008 guidelines, but even though the best results had been noticed among patients with QRS >150 ms, these guidelines failed to make specific recommendations based on QRS morphology and duration. Very important, though, is that no large scale trial mentioned at that time managed to demonstrate any benefi t in resynchronizing patients with normal or near normal (120-130 ms) QRS duration, even when echocardiographic elements of dyssynchrony were noticed1,14. Recent papers reinforce this statement adding that CRT may actually have deleterious effects in this group of HF patients (EchoCRT study)7. Other major trials like Resynchronization for Ambulatory Heart Failure Trial (RAFT)8, Multicenter Automatic Defi brillator Implantation Trial-Cardiac Resynchronization Therapy (MADIT-CRT)9, Cardiac Resynchronization in Heart Failure Study (CAREHF)10, Comparison of Medical Therapy, Pacing and Defi brillation in Heart Failure (COMPANION)11 were able to demonstrate greater benefi ts when CRT was performed in wide QRS population. A meta-analysis of these trials, which included also the Resynchronization Reverses Remodeling in Systolic Left Ventricular Dysfunction (REVERSE) study, proved important benefits in terms of morality and hospitalization for heart failure, in the QRS >150 ms patient population, regardless of HF severity12. Current information reveals there is no benefi t, or even there is a harmful effect when implanting a three chamber pace-maker when QRS duration is lower than 120-130 ms1. Regarding NYHA classification of HF, the REVERSE trial was the first one to notice that CRT has a reverse-remodeling effect in mildly or asymptomatic HF patients (when assessing left ventricular end systolic volume – LVESV in the CRT-ON group vs CRT-OF)12. Importantly, the reverse-remodeling effect was significantly lower in the non-LBBB pattern. Also, the study revealed that the longer the QRS duration, the greater the decrease in the LVESV. Another important aspect was the comparison between CRT-D and ICD alone, which was studied in the RAFT trial8. Overall, there was a better protection in terms of all-cause mortality, cardiovascular death and hospitalization (primary end point) offered by CRT-D implant (the differences were noticed only in the wide QRS complex (>150 ms), LBBB morphology and sinus rhythm). Similar conclusions were obtained in the MADIT-CRT trial, when comparing CRT-D vs ICD in patients with HF class I-II NYHA, QRS >130 ms9. A subanalysis of this study proved that only patients with LBBB morphology benefi t more from CRT-D vs ICD, whereas in the group presenting right bundle branch block (RBBB) or intraventricular conduction delay (ICVD) patterns there was no difference in terms of better protection between CRT-D and ICD9. The latest recommendations based on the newest trials are available from 2013 (2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy). These guidelines simplified the management of HFpatients, when speaking about CRT, and discouraged the use of the device in class I NYHA and non-LBBB pattern with QRS
THERAPY LIMITATIONS
It is estimated that 5-10% of all the HF population has indication for CRT. This represents a large number of patients, about 400/1.000.000 inhabitants/year in Europe14. Unfortunately, about one third of the implanted patients prove to be non-responders to therapy. We believe that this is mainly due to a lack of clear criteria able to predict response to therapy; next stands the technical impairment15. There is heterogeneity of mechanisms determining resynchronization success. As seen above, the present indications for CRT widely uses basic criteria in terms of LVEF, NYHA class and QRS duration, which apparently are insuffi cient when predicting the responders to therapy16. What is a responder? To answer this question, we must fi rst establish thetiming of evaluation. There is no consensus regarding this aspect, but there is a general opinion that at least 6 months must pass from the implant before we make an assumption17. There are at least three sets of parameters to have in mind. Firstly, of course, there are the morality-morbidity indicators21. Secondly, but maybe the most important, there are the clinical parameters: NYHA class (at least 1 class decease), 6 mwt (>50 m improvement), QOL, VO2 (>10 %). On the third position comes the echocardiographic evaluation (LVEF >5% and LVESV >10-15%)18. Interestingly, there is no direct correlation between QRS duration (narrowing) and the clinical/hemo-dynamical benefi t after CRT, according to literature19. According to these parameters, the responders to therapy are classifi ed in super- responders (EF improvement >20%, reduction of LVTSV > 30%), responders (EF improvement 5-20%, reduction of LVTSV 15-29%) and non-responders (EF improvement Indication related causes
– inappropriate patient selection
– narrow QRS, non-LBBB pattern, NYHA class I
– the absence of mechanical dissynchrony
– absence of contractile reserve
– presence of scar tissue at the place of the LV lead positioning
2. Patient related causes
– individual factors
– male gender
– ischaemic etiology
– RV dysfunction
– mitral regurgitation
– atrial fi brillation
– absence of complete myocardial revascularization before CRT implant
– other comorbidities
3. Device related/ Implant difficulties
– anatomical factors
– suboptimal lead positioning
– loss of LV capture (exit block, lead fracture)
– insufficient Bi-Ventricular pacing
– high cardiac rate / Atrial Fibrillation
– failure of device optimization (A-V, VV intervals)
Table 1. The summarization of CRT indications
FUTURE PERSPECTIVES
There are two major directions when seeking improvement in CRT: better patient selection and technique improvement. The first direction refers to a superior selection strategy capable of predicting greatest benefit from three-chamber pacing. Summarizing today’s understanding of this topic, LBBB remains the strongest substrate for resynchronization and patients with this pathology enjoy the best benefi t24. The MADITCRT study was able to identify, among the 191 superresponders to therapy, a number of six clinical characteristics signifi cantly related to procedural success: female gender, non-ischaemic etiology, QRS duration >150 ms, LBBB pattern, body mass index 99% biventricular pacing, experts recommendations, nowadays, refer to echoguided AV optimization early after implant using E and A waves and the use of synchronous biventricular pacing (0 ms VV interval) (2013 ESC Pacing and CRT Guideline)1. If no benefi t is observed, then echo-optimized VV interval should be tried out. Noninvasive ventricular mapping techniques are developed, like the multichannel mapping vest combined with CT imaging in the hope of better device programming13. New encouragement comes from using the newly developed automatic device optimization of AV and VV intervals by using complex algorithms. One such example, where this method is tested in comparison with standard approach, is the RESPOND CRT trial (Automatic Optiventrimization of Cardiac Resynchronization Therapy Using SonR — Rationale and Design of the Clinical Trial of the SonRtip Lead and Automatic AV-VV Optimization Algorithm in the Paradym RF SonR CRT-D)44. The SonR algorithm is based on weekly optimization of AV and VV intervals using an accelerometer able to measure changes in SonR signals (myocardial vibrations during isovolumetric contraction – which are proven to be correlated with the intensity of the fi rst sound and with cardiac contractility – related with dP/dT value)45,46. The method seems to be of great value as it has already shown superiority to conventional optimization techniques. Finally, we should mention that a special place is held by the remote monitoring device management, a method that is already in use in the USA and many European countries. Regarding ICD’s and CRT, remote monitoring proves to be of substantial aid when speaking in terms of long term survival and total hospitalization as shown in CONNECT and LATITUDE trials1,9,14.
CONCLUSIONS
One can say that the last decade brought resynchronization therapy from the state of timid trials to a reliable therapeutic method. Even though subject to many imperfections, it has proven to be a distinct healing direction and not a closed road. There are a lot of ongoing trials meant to improve both patients’ selection and implantation techniques that will surely alleviate the burden of HF disease. New ideas derived from better understanding of cardiac electrophysiology, supported by an incredible technical progress, form the background that could fundamentally shape the way we see CRT implant today.
Acknowledgements: ”This work received fi nancial support through the project entitled “CERO – Career profile: Romanian Researcher”, grant number POSDRU/159/1.5/S/135760, cofinanced by the European Social Fund for Sectoral Operational Programme Human Resources Development 2007-2013”.
Conflict of interest: none declared.
References
1. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J. 2013;34:2281–2329.
2. Cheuk-Man Yu et al. Cardiac Resynchronization Therapy, 2nd Edition. 2008; 28-43.
3. Sawhney, N. S.Randomized prospective trial of atrioventricular delay programming for cardiac resynchronization therapy. Heart Rhythm. 2004;122-133.
4. Vernooy, K. Left bundle branch block induces ventricular remodelling and functional septal hypoperfusion.Eur. Heart. J. 2005;3:91-98
5. Strik, M. Transseptal conduction as an important determinant for cardiac resynchronization therapy, as revealed by extensive electrical Electrophysiol. 2013;2-23.
6. Cazeau S, Leclercq C, Lavergne T. Multisite Stimulation in Cardiomyopathies (MUSTIC) Study Investigators. N Engl J Med. 2001; 344(12):873-80
7. Frank Ruschitzka, William T. Abraham et all. Echocardiography Guided Cardiac Resynchronization Therapy (EchoCRT) trial in patients with narrow QRS and ventricular dyssynchrony- Cardiac-Resynchronization Therapy in Heart Failure with a Narrow QRS Complex. N Engl J Med. 2013; 369:1395-1405.
8. Anthony S.L. Tang, George A. Wells, Mario Talajic. Cardiac-Resynchronization Therapy for Mild-to-Moderate Heart Failure. The New England Journal of Medicine. 2010; 363( 25): 2385-2395.
9. Hsu, J. C. Predictors of super-response to cardiac resynchronization therapy and associated improvement in clinical outcome: the MADIT-CRT (multicenter automatic defi brillator implantation trial with cardiac resynchronization therapy) study. J. Am. Coll. Cardiol.2012;59:2366-73.
10. Cleland JG, Daubert JC, Erdmann E, Freemantle N. The CARE-HF study (CArdiac REsynchronisation in Heart Failure study): rationale, design and end-points. Eur J Heart Fail. 2001;3(4):481-9.
11. Saxon, L. A.Infl uence of left ventricular lead location on outcomes in the COMPANION study QRS duration. J. Cardiovasc. Electrophysiol. 2009;84:1136-1144.
12. Linde, C. Long-term impact of cardiac resynchronization therapy in mild heart failure: 5-year results from the REsynchronization reVErses Remodeling in Systolic left vEntricular dysfunction (REVERSE) study.Eur. Heart J.2013;12:524-530.
13. Ping Jia, Charulatha Ramanathan, Raja N. Ghanem, Kyungmoo Ryu, Niraj Varma. Electrocardiographic imaging of cardiac resynchronization therapy in heart failure: Observation of variable electrophysiologic responses. Heart Rhythm. 2006 ; 3(3): 296–310.
14. Prinzen, F. W., Vernooy, K., Auricchio, A. Cardiac resynchronization therapy: state-of-the-art of current applications, guidelines, ongoing trials and areas of controversy. Circulation.2013;9:47-67.
15. Delnoy, P. P. Sustained benefi t of cardiac resynchronization therapy.J. Cardiovasc. Electrophysiol. 2007;12:36-65.
16. Wilton, S. B., Leung, A. A., Ghali, W. A., Faris, P., Exner, D. V.Outcomes of cardiac resynchronization therapy in patients with versus those without atrial fi brillation: a systematic review and meta-analysis (RAFT).Heart Rhythm.2011;130.
17. Yu, C. M. Tissue Doppler echocardiographic evidence of reverse remodeling and improved synchronicity by simultaneously delaying regional contraction after biventricular pacing therapy in heart failure. Circulation. 2002;104:448-450.
18. Seo, Y. The role of echocardiography in predicting responders to cardiac resynchronization therapy: results from the Japan Cardiac Resynchronization therapy registry Trial (J-CRT).Circ. J. 2011;43:57-80.
19. Mascioli, G. Electrocardiographic criteria of true left bundle branch block: a simple sign to predict a better clinical and instrumental response to CRT. Pacing Clin. Electrophysiol. 2012;121:54-61.
20. Gorcsan, J.Echocardiography for cardiac resynchronization therapy: recommendations for performance and reporting—a report from the American Society of Echocardiography Dyssynchrony Writing Group endorsed by the Heart Rhythm Society.J. Am. Soc. Echocardiogr. 2008;19:55-60.
21. Cleland, J. G..The effect of cardiac resynchronization on morbidity and mortality in heart failure.N. Engl. J. Med. 2005; 1322. Auricchio, A., Prinzen, F. W.Non-responders to cardiac resynchronization therapy: the magnitude of the problem and the issues.Circ. J. 2011;65:40-72.
22. C. Ginghină. Mic tratat de cardiologie. Ed. Academiei Române. 2010;679-737.
23. Stellbrink, C. Impact of cardiac resynchronization therapy using hemodynamically optimized pacing on left ventricular remodeling in patients with congestive heart failure and ventricular conduction disturbances.J. Am. Coll. Cardiol. 2001;38:21-36.
24. Gasparini, M. Long-term survival in patients undergoing cardiac resynchronization therapy: the importance of performing atrio-ventricular junction ablation in patients with permanent atrial fi brillation. Eur. Heart. J.2008;14:129-40.
25. Chung, E. S.Results of the Predictors of Response to CRT (PROSPECT) trial. Circulation.2008;54:56-82.
26. Strauss, D. G., Selvester, R. H., Wagner, G. S. Defi ning left bundle branch block in the era of cardiac resynchronization therapy. Am. J. Cardiol. 2011;50:1129-41.
27. Zareba, W. Effectiveness of cardiac resynchronization therapy by QRS morphology in the Multicenter Automatic Defi brillator Implantation Trial-Cardiac Resynchronization Therapy (MADIT-CRT). Circulation. 2011;104:44-52.
28. Abraham, W. T., Smith, S. A. Devices in the management of advanced, chronic heart failure .Nat. Rev. Cardiol. 2013;14-20.
29. Abraham, W. T. Cardiac resynchronization in chronic heart failure N. Engl. J. Med. 2002;11:1460-72.
30. Daubert, J. C. 2012 EHRA/HRS expert consensus statement on cardiac resynchronization therapy in heart failure: implant and follow-up recommendations and management. Europace. 2012;18:821-843.
31. Singh, J. P. Left ventricular lead position and clinical outcome in the multicenter automatic defi brillator implantation trial-cardiac resynchronization therapy (MADIT-CRT) trial. Circulation. 2011;128:2408- 2414.
32. Kandala, J. QRS morphology, left ventricular lead location, and clinical outcome in patients receiving cardiac resynchronization therapy. Eur. Heart J. 2013;12:46-50.
33. Chalil, S. Effect of posterolateral left ventricular scar on mortality and morbidity following cardiac resynchronization therapy. Pacing Clin. Electrophysiol. 2007;10:1201-9.
34. Prinzen, F. W., Hunter, W. C., Wyman, B. T., McVeigh, E. R. Mapping of regional myocardial strain and work during ventricular pacing: experimental study using magnetic resonance imaging tagging .J. Am. Coll. Cardiol. 1999;19:1279-86.
35. Bilchick, K. C. Cardiac magnetic resonance assessment of dyssynchrony and myocardial scar predicts function class improvement following cardiac resynchronization therapy. JACC Cardiovasc. Imaging. 2008;16:16-40.
36. Ypenburg, C. Impact of viability and scar tissue on response to cardiac resynchronization therapy in ischaemic heart fai. lure patients .Eur. Heart J. 2007;28:33-41.
37. van Gelder, B. M., Houthuizen, P., Bracke, F. A. Transseptal left ventricular endocardial pacing: preliminary experience from a femoral approach with subclavian pull-through. Europace. 2011;16:1119-30.
38. Ploux, S.Acute electrical and hemodynamic effects of multi-left ventricular pacing for cardiac resynchronization therapy in the dyssynchronous canine heart. Heart Rhythm.2014;11:119-25.
39. Rademakers, L. M., van Gelder, B. M., Scheffer, M. G., Bracke, F. A. Midterm follow up of thromboembolic complications in left ventricular endocardial cardiac resynchronization therapy. Heart Rhythm. 2014;9:122-136.
40. Leclercq, C. A randomized comparison of triple-site versus dual-site ventricular stimulation in patients with congestive heart failure. J. Am. Coll. Cardiol. 2008;15:1455-1462.
41. Echt, D. S., Cowan, M. W., Riley, R. E., Brisken, A. F. Feasibility and safety of a novel technology for pacing without leads. Heart Rhythm, 2006; 3:1102-6.
42. Bongiorni, M. G. Preferred tools and techniques for implantation of cardiac electronic devices in Europe: results of the European Heart Rhythm Association survey. Europace. 2013;15:1644-8.
43. Dekker, A. L Epicardial left ventricular lead placement for cardiac resynchronization therapy: optimal pace site selection with pressurevolume loops J. Thorac. Cardiovasc. Surg.2004; 127:1641-7.
44. Ellenbogen, K. A. Primary results from the SmartDelay determined AV optimization: a comparison to other AV delay methods used in cardiac resynchronization therapy (SMART-AV) trial: a randomized trial comparing empirical, echocardiography-guided, and algorithmic atrioventricular delay programming in cardiac resynchronization therapy. Circulation. 2010;124:191-192.
45. van Gelder, B. M., Bracke, F. A., Meijer, A., Lakerveld, L. J., Pijls, N. H. Effect of optimizing the VV interval on left ventricular contractility in cardiac resynchronization therapy. Am. J. Cardiol. 2004;93:1500-3.
46. Bogaard, M. D. Baseline left ventricular dP/dtmax rather than the acute improvement in dP/dtmax predicts clinical outcome in patients with cardiac resynchronization therapy. Eur. J. Heart Fail. 2011;13:1126-1132.
 This work is licensed under a
This work is licensed under a