Ovidiu Chioncel1, Gabriel Tatu-Chitoiu2, Ruxandra Christodorescu3, Ioan Mircea Coman1, Dan Deleanu1, Dragos Vinereanu4, Cezar Macarie1, Marisa Crespo5, Cecile Laroche6, Thierry Fereirra6, Aldo Maggioni7, Gerasimos Filippatos8
1 “C.C.Iliescu” Emergency Institute for Cardiovascular Diseases, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania
2 Floreasca Emergency University, Bucharest, Romania
3 ASCAR Clinic, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania
4 Emergency University Hospital, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania
5 Unidad de Insuficiencia Cardiaca Avanzada y Trasplante Cardiaco, Complexo Hospitalario Universitario A Coruna, CHUAC, La Coruna, Spain
6 EURObservational Research Programme, European Society of Cardiology, Sophia-Antipolis, France
7 ANMCO Research Center, Florence, Italy
8 Athens University Hospital Attikon, Athens, Greecea
INTRODUCTION
Heart failure (HF) is a clinical syndrome that represents the common manifestation of diverse cardiac and noncardiac pathologies. HF represents a condition with a negative impact on both the individual, because of lost years of life and by altering the quality of life, and on the health system, by raising the financial and social costs. In spite of increased survival, HF prevalence will continue to increase because of the ageing population and the increase in survival following acute conditions (myocardial infarction, acute valvular diseases). Recent data of the European Heart Failure Association has shown that 26 millions of people have been diagnosed with HF, worldwide, and 3,6 million are newly diagnosed each year, only in Europe1. In Romania, the picture is even more dramatic – a percentage as high as 4,7% of the general population above 35 years, are diagnosed with HF2. Epidemiological data on HF is missing in many countries, because of the absence of relevant observational studies, to capture the incidence, prevalence, prognosis and main causes for HF. The understanding of the epidemiology and the clinical characteristics of HF in a certain population is key issue in improving prognosis. Randomized clinical trials bring important epidemiological information, but its generalization and applicability are limited by the very strict inclusion and exclu-sion criteria. Even though registries don’t have such limitations and probably refl ect the global population with HF in a certain geographical area, there are major differences at both continental and regional level, in regard to the severity, etiology and HF management3. There have been several registries and trials in Europe, in acute or chronic HF patients, but with several limitations, regard to the representatives for each country, the degree of data completion and especially, to 1-year follow-up4-6. The European HF-Long Term Registry is a permanent registry of the European Society of Cardiology (ESC)7. Its main objective was to describe the clinical epidemiology of ambulatory and hospitalized HF patients and the diagnostic and therapeutic procedures applied to these patients in Europe, including the HF management programs organization7. The present paper aims to characterize in terms of demography, clinical presentation, biology, and treatments, the subset of patients with HF enrolled in Romanian centers. Furthermore, other important objective of the study is to evaluate the 1-year prognosis of acute and chronic HF patients, in the subgroup of Romanian patients and to compare them with the rest of patients, enrolled in the registry.
METHODOLOGY
Study characteristics
The ESC HF-LT Registry is a prospective, multicenter, observational study, which enrolled patients with HF in 211 cardiology centers from 21 countries affi liated to the (ESC). Center selection was made based on geographic representatives and accounting for medical facilities available at national level. In each country, for every 2 million inhabitants, one investigational center was assigned. At the moment of the present analysis, a total number of 12440 patients were enrolled, starting with May 2011, and of these, 380 patients had been enrolled in Romania.
Inclusion criteria
All ambulatory patients with HF evaluated in clinics and those hospitalized for acute HF (either previously diagnosed, or de novo HF), for which intravenous therapy was required, were included. To facilitate consecutive enrolment, patients were enrolled in the registry on a one-day-per-week basis. One 12 months follow up visit was mandatory to collect morbidity and mortality data (death, re-hospitalization). A telephone call visit was accepted to replace the clinical visit, if thepatient was unable to arrive at the reference centers. During the course of the year patients were followedup according to the usual practice of each center. There were no specific exclusion criteria, except age (which had to be above 18 years). The study was approved by each local Ethics Committee, according to the local rules of each participating country. The data on the study were not collected before detailed information was given to the patient and the informed consent form was signed. At 1-year follow-up, the data of the patients enrolled during the main part (data of study patients from the best 12 consecutive months, for each country) was analyzed.
Participating centers
The patients were enrolled in the following countries and regions: Lithuania and Sweden (Northern countries); Bosnia & Herzegovina, Bulgaria, Czech Republic, Hungary, Latvia, Poland, Romania and Slovakia (Eastern countries); Austria and France (Western countries); Greece, Italy, Portugal, Serbia, Slovenia, and Spain (Southern countries). There were 10 centers in Romania: 3 in Bucharest, 1 in Timisoara, 1 in Galati, 1 in Brasov, 1 in Slobozia, 1 in Iasi, 1 in Targoviste and 1 center in Focsani. (Appendix 1).
Statistical analysis
Categorical variables were expressed as numbers and proportions (N, %) and continuous variables as mean or median, based on distribution (mean, SD, median, interquartile ranges). All results were presented for regions (Romania vs. other countries in EU) and for subgroups (acute vs. chronic HF). Categorical variables were compared by the X2 test and continuous variables by a non-parametric test (Kruskal-Wallis test). Demographical and clinical characteristics and type of treatments were also compared between the HF cohort of Romania (RO) and the rest of the participating countries (other EU). Plots of Kaplan-Meier curves for time to all-cause death, time to admission to hospital for HF and time to all-cause death or HF hospitalization were performed. In addition, these plots were divided into outpatients with chronic HF and in patients with acute HF. A p-value
RESULTS
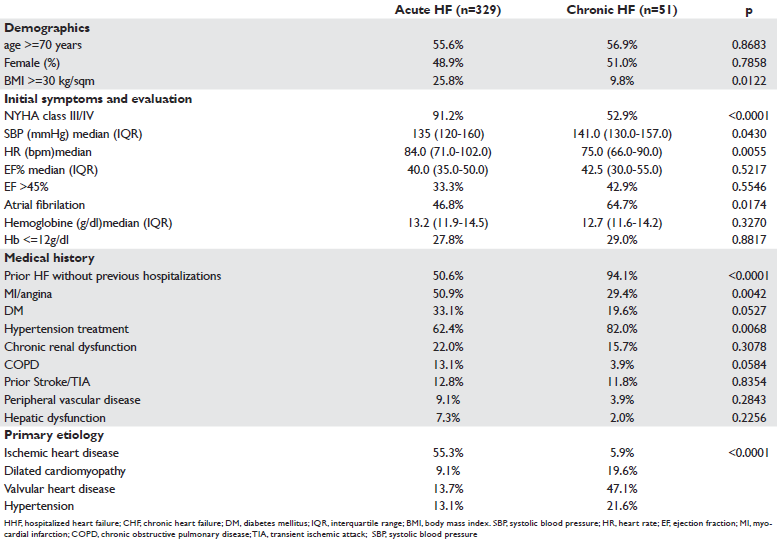
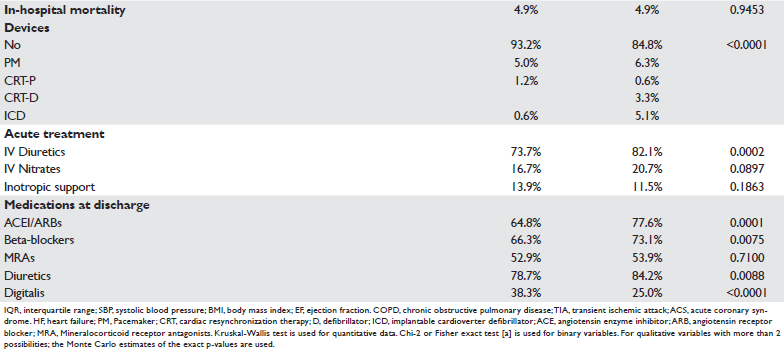
During the enrolment period 12440 patients were enrolled in the registry. Of these, 380 patients were enrolled in Romania, representing 3.7% of the total number of patients. With regard to the clinical form of HF, 51 patients had chronic HF and 329 patients had hospitalized HF. The differences in demographic, clinical, biological characteristics between the two populations are presented in Table 1. Compared to patient with chronic HF, hospitalized HF patients have lower SBP, lower EF and more frequent ischemic etiology. Also, patients with acute HF are more frequently in NYHA classes III and IV (91.2% vs 52.9%; p<0.0001). In-hospital mortality of acute HF patients was 4.9%. 1-year follow-up analysis revealed significant differences regarding the adverse event rate (death, HF hospitalization, death or hospitalization) between the chronic HF and hospitalized HF patients, enrolled in Romania. 1-year mortality in patients hospitalized for acute HF was 24.4% and 6% in chronic HF. A percentage of 15.2% of acute HF patients are readmitted at 1 year because of HF and 8.9% of patients with chronic HF have a readmission due to HF, when analyzed at 1-year follow-up (Table 2). The Kaplan-Meyer curves show that these differences become larger as the duration of patient’ followup increases (Figures 1, 2 and 3). Regarding the comparison between patients enrolled in Romania and those in other participating countries, this is differentially presented for patients with acute HF (Table 3) and those with chronic HF. Generally, the clinical characteristics at presentation are similar between patients with acute HF enrolled in Romania and patients enrolled in the rest of the participating countries. There are differences on female sex prevalence (Table 1) and the proportion of comorbidities, anemia, respiratory disease, less frequent in the Romanian population. The frequency of clinical forms of acute HF is also similar. In-hospital mortality was identical (4.9%). Significant differences exist between the rate of device treatment, which is considerably lower in Romania. Also, for the neurohormonal medication at discharge, o smaller proportion of Romanian patients received beta-blockers (BB) and angiotensin conversion enzyme inhibitors (ACEI) as compared to other European countries. Digoxin use at discharge is more frequent in Romania. 1-year mortality is similar (24.4% vs 28.1%; p=0.157), but the number of patients readmitted because of HF is smaller in Romania, as compared to other participating countries (15.2% vs 27.1%; p<0.0001). As regard to chronic HF patients, the Romanian population is older and female sex is more prevalent.
As compared to other countries, chronic HF patients enrolled in Romania have o higher prevalence of atrial fi brillation (64.7% vs 37.4%; p<0.0001) and valvular etiology (47.1% vs 8%; p<0.0001). No significant difference was found between the neurohormonal medication between patients with chronic HF in Romania and patients in other countries. Also, the adverse event
rate at one year was similar for patients enrolled in Romania, as compared to other countries. 1-year mortality in chronic HF Romanian patients was 6%, while in other countries was 8% (p=0.757).
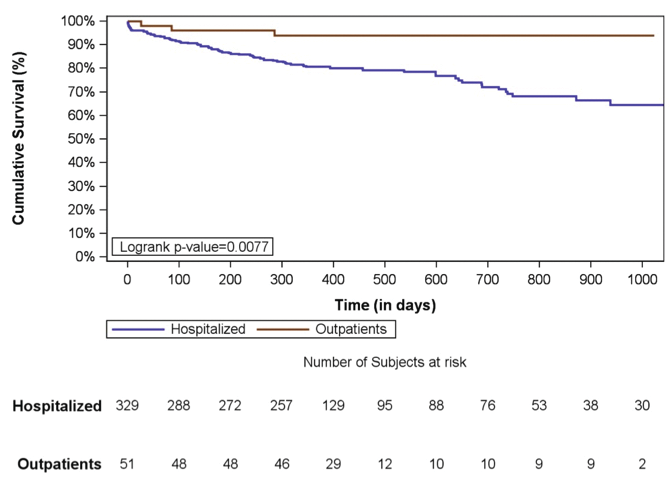
Figure 1. Kaplan-Meyer survival curves for all-cause mortality in patients with acute hospitalized HF and chronic ambulatory HF; data from Romanian subgroup.
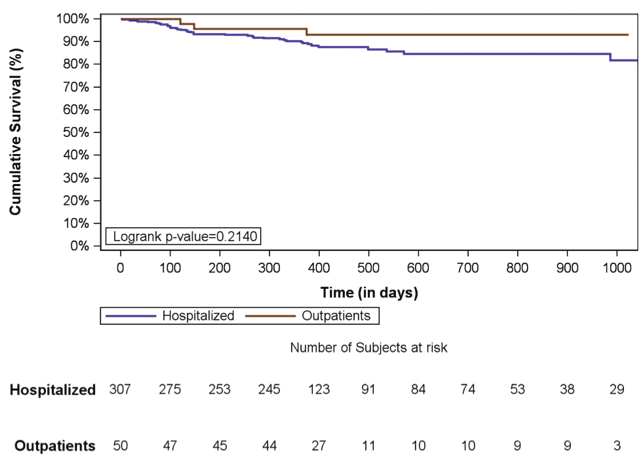
Figure 2. Kaplan-Meyer survival curves for HF readmissions in patients with acute hospitalized HF and chronic ambulatory HF; data from Romanian subgroup.
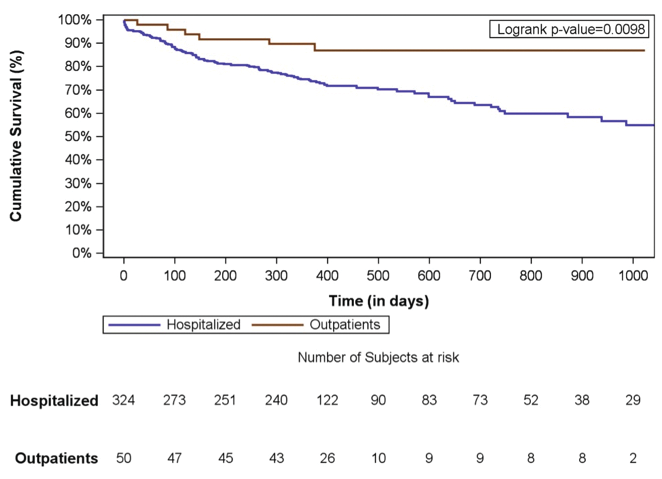
Figure 3. Kaplan-Meyer survival curves for all-cause mortality or HF readmissions in patients with acute hospitalized HF and chronic ambulatory HF; data from Romanian subgroup.
Table 1. Heart Failure Long-Term analyses for Country Romania; baseline characteristics – Country Romania
DISCUSSION
This data represents the most recent epidemiological European experience as regard to observational studies. The ESC HF LT registry is one of the few observational studies with 1-year follow-up for both patients with acute HF and those with chronic HF. Importantly, the response rate at 1 year follow-up was above 95%. Although Romania has a good coverage and a good epidemiological knowledge of population of acute HF patients, there hasn’t been so far a national registry with rigorous follow-up after hospitalization2,8,9. Similar to other European countries and to the previous registry of the European Society of Cardiology, the classification of patients with HF in two types – chronic (in ambulatory practice) and acute HF (that requires hospitalization) has clinical and prognostic value6. There are significant differences regarding 1-year mortality nd the readmission rate between the two categories, regardless of geographical area, observational study or year of enrollment. For a population of about 20 million inhabitants, Romania had a medium enrollment rate, with 380 HF patients, representing 3.7% from the total number of enrolled patients. Interestingly, most Romanian patients had acute HF, which may be explained by the type of ambulatory practice of the affi liated hospitals in Romania. Importantly, there were no significant differences for 1-year mortality between HF patients in Romania and those enrolled in other countries. Like in other countries, 1-year mortality was different between patients with acute HF and those with chronic HF (22.4% vs 6%). Also, as for the number of patients requiring hospitalization for any cause during the 1-year follow-up, there were differences between patients with acute and chronic HF (26% vs 22%). It is worth to note that regardless of region or the type of HF patients, more than half of re-admissions are not related to worsening HF. This should be carefully noticed when strategies to lower re-hospitalisation ratse are considered. Many of re-admissions are non-cardiac in origin and are due to worsening of non-cardiac comorbidities, as theese are very frequent both in patients with acute and chronic HF. Thus, identifi cation and treating comorbidities remain an important target during hospitalization and represent a component of comprehensive management directed to decrease post-discharge outcomes. Although, no substantial differences in 1-year mortality have been detected between patients enrolled in Romania and in other counties, the rate of 1-year re admissions was considerably lower in Romania compared to other countries. This may be explained by the absence of universally accepted criteria for HF admission, as well as by different pshychological and social thresholds for hospital admission infl uenced by the differences in cultural perception of severity. For the patients hospitalized in Romania, the frequency of which received the guideline recommended therapy at discharge, was lower than in other European countries10. Although in Romania, there has been a continuous increase in prescription of evidence based therapies2, there probably still exist a large number of patients that are eligible to receiving such medication. From a Romanian perspective, by analyzing two epidemiological studies that took place at 5 years apart (Table 5), an increase in the prescription of oral medications at discharge can be noticed. This is mainly true for beta-blockers, for which there has been an absolute increase of 10%. By using this percentage to the proportion of HF patients hospitalized in Romania and by knowing that the number needed to treat with BB to save a life is 15, we can estimate that approximately 1400 HF patients had a survival benefi t by increasing the rate of BB use in this 5-year interval11. Unfortunately, the rate of use of HF related devices and interventional procedures, although is increasing, is still unacceptably low, and reflect lack of these facilities and probably overall economic development. National programs to implement larger in-hospital utilization of these procedures are needed.
Table 2. 1-year FU Outcomes – Heart Failure Long-Term analyses for Country Romania
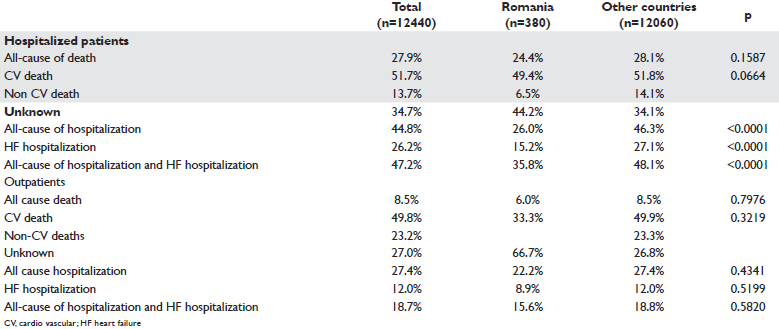
Table 3. Comparison between hospitalized patients with heart failure in Country Romania and other countries participating in ESC-HF Long Term registry – Country Romania
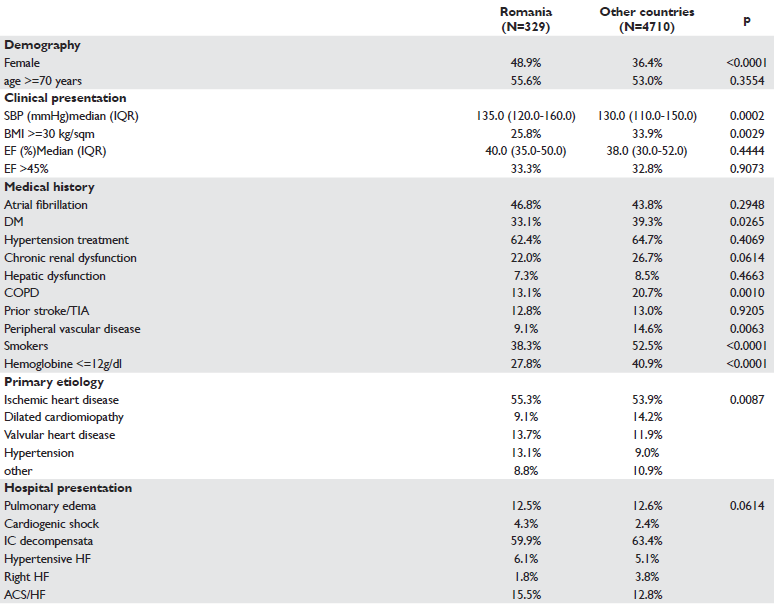
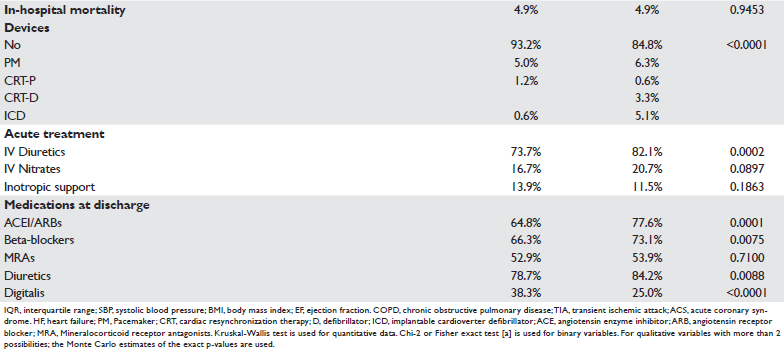
Table 4. Comparison between CHF patients in Country Romania and other countries participating in ESC-HF long term registry – Country Romania
LIMITATIONS
ESC HF LT registry has enrolled patients capable of understanding and signing the informed consent. This fact, limited the enrollment of patients that are in a critical state at admission, who not have the capacity to sign. Also, patients who died in the first 24 hours (criteria used to defi ne hospitalization) were not enrolled, fact which may underestimate in-hospital mortality. Another methodological request of the registry was the ability to be contacted and to be willing to participate in a follow-up visit. All these limitations, which actually represent very rigorous methodological criteria, may contributed to a lower proportion of severe patients, and to an adverse event rate smaller than expected. Another important limitation is that the enrollment rate varied significantly between participating centers.
CONCLUSIONS
Rigorous epidemiological research represents the mainstay for precise knowledge of a certain pathology at national and regional level. HF is a multi-event disease and accurate characterization of these patients is critical for improving long-term outcomes. The ESCHF- LT registry confi rms that patients with acute HF have a worse prognosis than patients with chronic HF, regardless of geographical region, and for the hospitalized HF patients, risk to die extends beyond the period of hospitalization. In Romania, HF represents a severe clinical condition that is associated to a high rate of death and re-hospitalizations, which is particularly dramatic for acute HF patients, meaning that 36% of patients either die or are re-hospitalized during 1-year follow-up.
Conflict of interest: none declared.
References:
1. Ponikowski, P., et al., Preventing disease and death worldwide ESCHFA white paper. Available from: http://www.escardio.org/static_fi le/Escardio/Subspecialty/HFA/WHFA-whitepaper-15-May-14.pdf.
2. Macarie, C. and O. Chioncel, Studiul românesc de prevalenţă a insuficienţei cardiace în populaţia arondată medicilor de familie, in Progrese in cardiologie. 2007. p. 311–27.
3. Ventura, H.O. and K.K. Gaddam, Geographic variations of acute heart failure syndromes: the importance of clinical registries. Am Heart J, 2011. 162(1): p. 1-2.
4. Nieminen, M.S., et al., EuroHeart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J, 2006. 27(22): p. 2725-36.
5. Mebazaa, A., et al., Short-term survival by treatment among patients hospitalized with acute heart failure: the global ALARM-HF registry using propensity scoring methods. Intensive Care Med, 2011. 37(2): p. 290-301.
6. Maggioni, A.P., et al., EURObservational Research Programme: regional differences and 1-year follow-up results of the Heart Failure Pilot Survey (ESC-HF Pilot). Eur J Heart Fail, 2013. 15(7): p. 808-17.
7. Maggioni, A.P., et al., Are hospitalized or ambulatory patients with heart failure treated in accordance with European Society of Cardiology guidelines? Evidence from 12,440 patients of the ESC Heart Failure Long-Term Registry. Eur J Heart Fail, 2013. 15(10): p. 1173-84.
8. Chioncel, O., et al., The Romanian Acute Heart Failure Syndromes (RO-AHFS) registry. Am Heart J, 2011. 162(1): p. 142-53 e1.
9. Antohi, E.-L., et al., Relation between comorbidities and use of evidence based therapies in patients with in-hospital heart failure; data from the IHHF RO study. European Journal of Heart Failure, 2013.
10. McMurray, J.J., et al., ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J, 2012. 33(14): p. 1787-847.
11. Chatterjee, S., et al., Benefi ts of beta blockers in patients with heart failure and reduced ejection fraction: network meta-analysis. BMJ, 2013. 346: p. f55.
 This work is licensed under a
This work is licensed under a