Bruno R Nascimento1,2,3, Luisa C C Brant1, Diego N Moraes1, Antonio L P Ribeiro1,3
1 Serviço de Cardiologia e Cirurgia Cardiovascular – Hospital das Clínicas da Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil
2 Serviço de Hemodinâmica – Hospital das Clínicas da Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil
3 Departamento de Clínica Médica da Faculdade de Medicina – Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil
* To cite: Nascimento BR, Brant LCC, Moraes DN, et al. Heart 2014;100:1743-1749.
** First published in Heart [Heart 2014;100:22 1743-1749.] and reproduced with permission. Copyright restrictions apply.
INTRODUCTION
Global Health, formerly referred to as ‘International Health’,1 involves numerous aspects of health policies,
epidemiology, prevention, diagnosis and therapy for neglected diseases and is not restricted to low resource regions. It is supported by four main bases: (A) clinical decision based on data and evidence; (B) population-based rather than individual focus; (C) social goals; (D) preventive rather than curative care.2 Broadly, Global Health has been defined as “worldwide improvement of health, reduction of disparities and protection against global threats that disregard national boundaries”.3 The Global Health Education Consortium highlights its relation to “health practices, policies and systems, stressing the differences rather than commonalities between countries”.4 Its mission has been proposed by the US Institute of Medicine as: “fulfilling society’s interest in assuring conditions in which people can be healthy”.5 Global Health exceeds the boundaries of infectious or neglected diseases and underdeveloped areas and focuses on multidisciplinarity and interdisciplinarity, embraces prevention, seeks equity and emphasises health as a public good, beyond borders.
The aim of this paper was to assess the contribution of ‘Heart’ to Global Health knowledge related to cardiovascular diseases (CVDs), reviewing articles published in the past 2 years (from May 2012 to April 2014). Given the breadth of important topics, we ca tegorised our review into studies relevant to understanding CVD epidemiological transition, trends in morbidity and mortality, aspects of vascular diseases and non-CVD, cardiovascular manifestations of selected communicable diseases, other CVDs and cardiovascular health promotion.
EPIDEMIOLOGICAL TRANSITION
In the last century, with the improvement in health conditions, the world has lived a change of the predominant
causes of death from infectious diseases and nutritional deficiencies to non-communicable diseases (NCDs), such as cancer, diabetes, respiratory and cardiovascular diseases.6,7 This ‘epidemiological transition’ resulted from population aging—due to lower fertility rates and greater life expectancy—and the rising rates of urbanisation that, along with globalisation, favoured health behaviours that raised the burden of cardiovascular risk factors for ischaemic heart di sease (IHD) and stroke, the main causes of morta lity worldwide.7 Indeed, equations that integrate age, risk factors and health behaviours in a variable defined as ‘cardiovascular risk age’ have been proposed as practical and intuitive methods for communicating about car diovascular risk.8 Although the epidemiological transition has already occurred in high-income countries (HICs), like the USA and Western Europe, it is happening in different paces in low and middle-income countries (LMICs),9 commonly affecting individuals at premature ages and from poorer ethnic groups or regions.9,10 In the Sub-Saharan Africa, for example, CVDs such as rheumatic heart disease and HIV-related disorders are highly prevalent, although hypertensive heart disease and stroke have more recently became established causes of death and disability, resulting from poorly controlled hypertension.11 Recent WHO STEPwise approach to surveillance (STEPS) surveys suggest that the rates of CVD risk factors are still lower in these countries than other regions of the world—but should not be considered low—although the rates of IHD remain low. In countries where population aging has evolved, such as in South America,10,12 unhealthy lifestyles became more common, resulting in higher rates of atherosclerotic CVD, that occurs in more premature ages when compared with HIC.7 The efforts to prevent, diagnose and treat IHD, stroke and their risk factors delay the morbimortality from these diseases, which will then usually occur at ages above 50 years.7 Data from Nordic countries registries show that despite the aging process, such efforts still result in steep declines in age standardised CVD mortality.13
CURRENT MORBIDITY AND MORTALITY TRENDS
It is estimated that CVDs account for about a third of all deaths worldwide, being also responsible for a great number of disabilities and significant economic impact. In the Americas, a study showed that from 2000 to the present, CVD comprised 33.7% of recorded deaths (with 42.5% attributed to IHD), with higher rates in women.12 The 20% mortality reduction in the continent during this period has mainly occurred in HICs—around 50–80%—and mortality and hospitalisation rates are decreasing.14,15 However, discrepancies can be observed across nations and even in regions of the same country,10 which may reflect inequality in access to healthcare and preventive policies.9 The median of CVD death rates of American LMICs, for example, is 56.7 higher compared with HICs (Figure 1)12 and a study conducted in the same time frame in Brazil showed that, although falling, death rates are still higher than those observed in wealthier countries.10 In China, on the other hand, IHD mortality increased since 1984, driven by persistent smoking, high cholesterol levels and population aging.9
VASCULAR AND NON-VASCULAR DISEASES
Health behaviours and risk factors
Most of the CVD burden can be attributed to a small number of lifestyle factors9—diet, exercise practices, smoking and alcohol consumption. Among these health behaviours, the regional and social peculiarities of dietary habits are known to have a significant cause effect relationship with CVD. For example, higher serum concentrations of n-3 polyunsaturated fatty acids, common in Asian diets, contributed to the lower incidence of coronary calcification in Japanese men in a 5-year follow-up cohort.16 Similarly, in a Danish cohort a negative dose-response trend was observed between tissue concentrations of n-3 polyunsaturated fatty acids and the new onset of atrial fibrillation (AF).17 The role of higher calcium intake on cardiovascular risk has also been under evaluation. In 1206 patients of the German KAROLA (Langzeiterfolge der KARdiOLogischen Anschlussheilbehandlung) study, after an acute cardio vascular event, higher baseline serum calcium levels were associated with higher risk of all cause (HR=2.39) and
cardiovascular (HR=2.76) death at 8 years.18 Paradoxically, in another large German population-based cohort, higher total and dairy dietary calcium intakes reduced the 11-year risk of myocardial infarction in 23 980 event-free participants, while stroke risk and CVD mortality were not affected.19 Tailored salt restriction has been established as an evidence-based measure for hypertension, and also in particular situations—such as chronic kidney disease—and specific ethnicities.20 Smoking habits have also been given attention in Global Health research. Cultural habits related to smoking seem to have similar deleterious effects, but are still under investigation. In a cross-sectional study in a large Iranian cohort, for example, the association of water-pipe smoking and CVD prevalence was consistently shown (HR=3.75), whereas chewing nass did not have the same effect.21
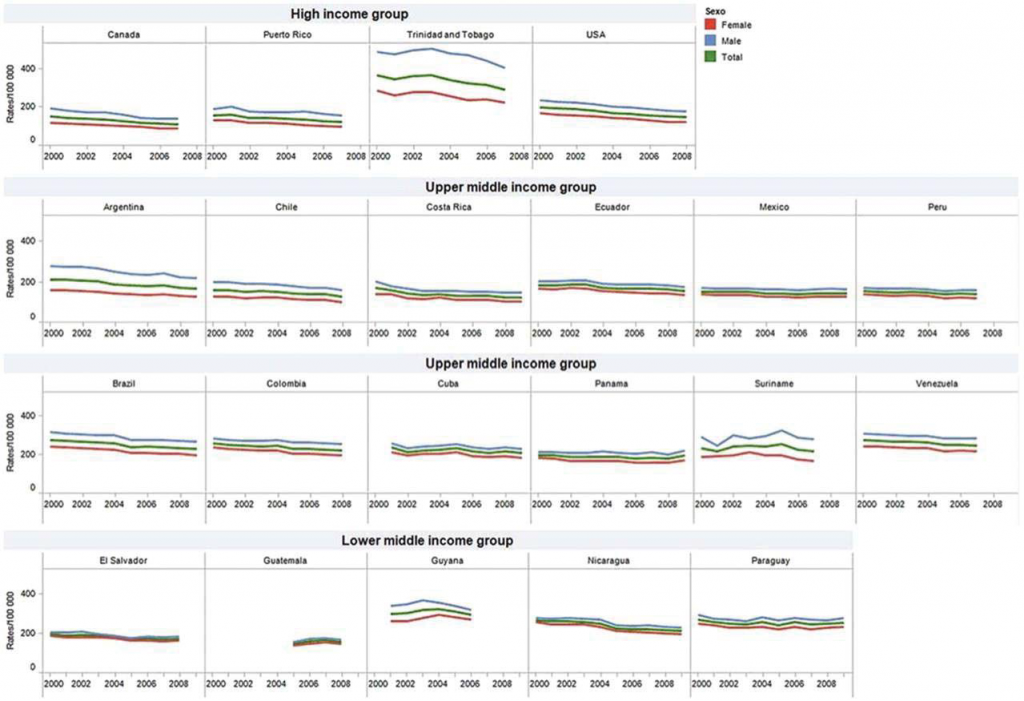
Figure 1. Trends in mortality due to cardiovascular diseases (ICD-10 I00–I99) (age-adjusted rates/100 000). Selected countries (upper, upper middle and lower middle income groups) in the Americas, 2000 to latest available year (adapted from de Fatima Marinho de Souza et al12).
Environmental factors
Although less established, environmental characteristics must also be discussed in CVD epidemiology rounds. An example is cardiovascular response to extreme temperatures. Cold weather was associated with increased risk of myocardial infarction in different populations and this effect seems to be affected by cultural habits, such as behavioural protection.22 Epidemiological evidence from a recent surveillance in five Chinese cities demonstrated that extremely hot or cold temperatures increased IHD mortality (18% and 48%, respectively), in a non-linear way.23 Air pollution is also implied as a trigger for increased all-cause mortality and cardiovascular mortality,24 with pronounced effects demonstrated in postmenopausal woman.25 A recent meta-analysis of 29 studies supported that slight increases in particulate matter have an inverse relation with heart rate variability, a marker of worse cardiovascular prognosis.26 Similarly, exposure to biomass fuel seems to be associated with higher prevalence of carotid plaques (OR=2.6).27
Ethnic factors
The ethnic composition of populations in also implied in differences in CVD burden and outcomes, which can be attributed to biological, cultural, healthcare and social issues.28 For example, it has been suggested that Africans and/or Asians might have higher IHD mortality due to intrinsic biological aspects. In Asian Indians, a positive association between high cytomegalo-virus antibodies titles and increased risk of IHD was found, suggesting that infectious disease prevalence may be involved in higher CVD mortality in this population.29 In the UK, the increased coronary mortality among south Asian minorities was related to a higher incidence of IHD, with similar case fatality.30 These findings are supported by a meta-analysis that strongly showed that south Asians have higher mortality because of higher incidence of IHD, even though their individual prog nosis appeared to be better than that of white populations after adjustment for confounding factors.31
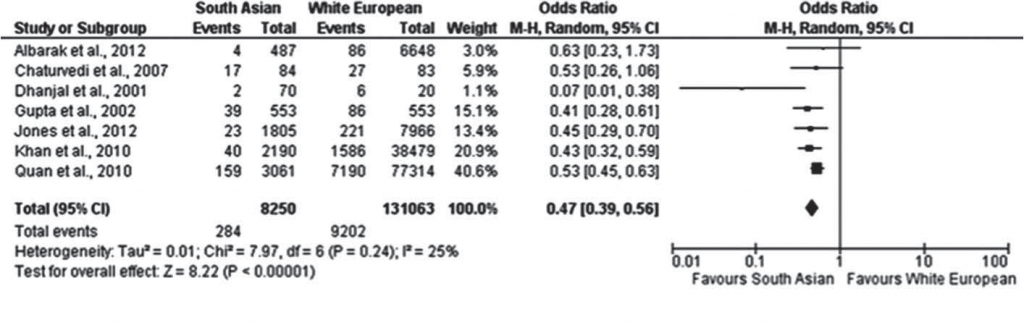
Figure 2. Forest plot of peripheral artery disease prevalence in coronary artery disease comparison studies, between South Asians and White Europeans (adapted from Sebastianski et al34).
This subpopulation also had a higher risk for stroke (OR=1.67) in another British cross-sectional study involving 6292 patients with AF.32 Paradoxically, in a Canadian cohort involving patients with newly diagnosed hypertension, south Asians had lower risk of death and adverse cardiovascular outcomes, despite having lower incomes and higher rates of hypertension compared with white patients.33 Peripheral artery disease prevalence was also significantly lower among South Asians in a meta-analysis of 15 studies (Figure 2).34 Thus, a combination of metabolic, behavioural and environmental factors are implied in these ethnic particularities, requiring earlier preventive interventions.30 Ethnic diversity and its multifactorial mediators may also influence the predictive power of cardiovascular risk scores: neither Framingham nor QRISK performed consistently well in the three ethnical groups evaluated in a primary care Londoner cohort.35 The understanding of ethnic differences in health is beneficial to minorities and it contributes to decreasing health inequalities in a large sense.
CARDIOVASCULAR MANIFESTATIONS OF SELECTED COMMUNICABLE DISEASES
Besides IHD, the burden of other CVDs is also different between HICs and LMICs, with the latter dealing with severe cardiac consequences of endemic diseases, typical of their social and economic situation. In Africa, the impact of HIV infection is considerable, especially in the sub-Saharan region, influencing CVDs. In the Heart of Soweto Study, 10% of patients with newly diagnosed CVD were HIV positive, and the most common HIV-related presentations were cardiomyopathy, pericardial disease and pulmonary hypertension.36 HIV infection also seems to be associated with sudden cardiac death and its burden is increased by the common association with Mycobacterium tuberculosis infection. In HIV-infected patients in sub-Saharan Africa, close to 100% of pericardial effusions are due to tuberculosis; the association with myopericarditis is common and an important part of it (40%) evolves with decreased LVEF.37 A factor of major relevance is that HIV-related cardiomyopathy is more common with increased immunosuppression and viraemia, whereas adequate antiretroviral therapy lowers its prevalence,38 implying that controlling this disease may reduce its CVD consequences. Increased access to medical care and to echocardiography in some parts of the continent has led to the recognition of endomyocardial fibrosis in areas in which the disease had not been previously reported. Although advances in establishing the epidemiology and improving clinical diagnosis and management through medical therapy and improved surgical techniques have been made, unfortunately the mortality related to this disease is still considerable.39
OTHER CARDIOVASCULAR DISEASES
In a review about heart failure (HF) in Africa, it was observed that the main aetiologies that resulted in acute decompensated HF were hypertension, cardiomyopathy and rheumatic heart disease, comprising 90% of cases, a pattern that contrasts with the predominance of IHD in North America and Europe (Figure 3). In this continent, HF affected mainly the young (mean age=52 years), without sex predominance, and is associated with 18% mortality at 6 months, similar to what has been observed in non-African HF registries, suggesting that HF has a dire prognosis independently of the region.40 In Tanzania, a study showed that patients hospitalised by HF were younger and their mortality was higher when compared with developed countries.
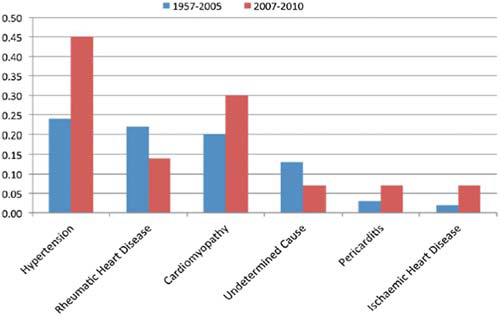
Figure 3. Differences in the proportion of causal factors for heart failure in sub-Saharan Africa during the periods 1957–2005 and 2007–2010 (adapted from Sliwa and Mayosi40).
The aetiologies of HF are becoming progressively similar to wealthier countries, with an increase of hypertension and a decrease of rheumatic heart disease.41 Hypertensive cardiomyopathy, once considered rare in sub-Saharan Africa, also seems to be a growing epidemic in this area and, without appropriate control, it will probably result in new patients with HF, and it might increase the incidences of IHD, AF and stroke.42 Concerning peripartum cardiomyopathy, a recent South-African study with 176 patients showed that 26% had a poor outcome (death, LVEF <35% or sever symptomatic HF), what translates in great impact, especially if it is considered that this disease affects women in reproductive age. The predictors of worse prognosis were functional class, LVEF and LV end diastolic dimension.43 A summary of Global Health articles published in Heart in the past two years about other non-vascular diseases is in Table 1.
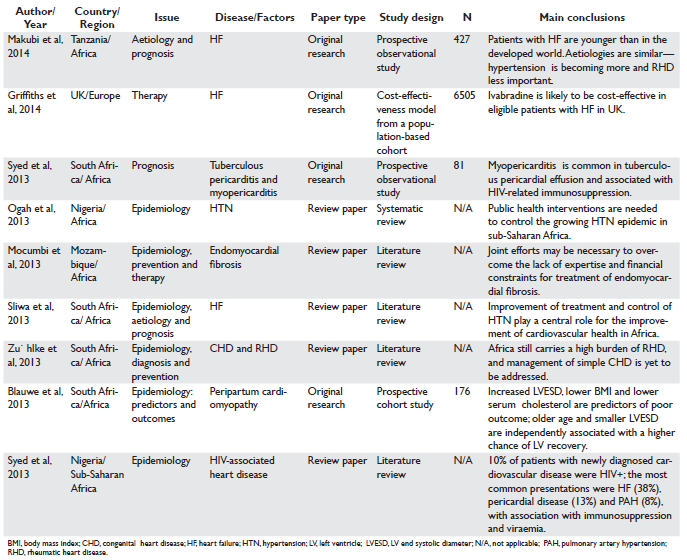
Table 1. Main Global Health articles published in Heart from May 2012 to April 2014 about other non-vascular diseases
HEALTH PROMOTION, PREVENTION AND CARE OF CARDIOVASCULAR DISEASES
The magnitude of the problem regarding CVD in the current context of Global Health makes facing these diseases a health priority. The challenge faced by HICs is to maintain their achievements in CVD mortality rate reduction conquered in the last decades9,12 and also to reduce inequities, by promoting this decline in specific minority groups that suffer the greatest burden of CVD in these countries, such as the African Americans in the USA and the South Asians in the UK.30,44 LMICs live a different reality: CVD mortality rate is increasing in some countries and, although in others it has decreased, the absolute numbers are increasing, mainly due to population aging.12 Therefore, lessons learned worldwide should be adapted to each country’s reality. To choose where to act, policy makers have evidence revealing that the reduction in IHD mortality rates in HICs are 45–75% a result of risk factor control and 25–55% due to treatment interventions.6,9 It is clear that policies should focus on population-wide
strategies, as well as aim at raising public awareness, empowering people to be partners in their own care; enhancing economic and environmental policies and orientating health systems capacities (Box 1).11,45,46 To confront the unhealthy behaviours that lead to the growing incidence of CVD, marketing practices can be used to stimulate physical activity and healthy eating. 6,9,45 Regulating contents of high-energy foods, such as sugary drinks, and subsidising fruits, vegetables and wholefoods can promote healthier diets.6,9,45 Smoking bans and increased taxation of tobacco and alcohol have been proven to reduce CVD.6,47 In the Netherlands, the working-place smoking ban significantly decreased the rates of out-of-hospital sudden cardiac deaths by about 12% (Figure 4),48 while in Brazil about 420000 deaths are estimated to have been prevented due to tobacco reduction over the years 1989–2010.49
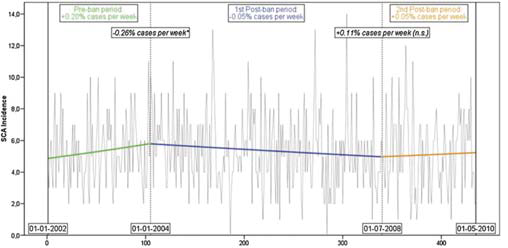
Figure 4. Absolute number of observed cases (grey lines) and trends in the incidence (bold lines) of out-of-hospital sudden circulatory arrest between 1 January 2002 (week 1) and 1 May 2010 (week 435). Vertical dotted lines represent the introduction of the two smoking bans, in week 105 (workplace ban) and week 340 (hospitality sector ban), respectively. The text boxes display the slopes (regular font) and changes in slopes (italic) of the unadjusted Poisson regression model. *Significant change in slope (p<0.05) (adapted from de Korte-de Boer et al48).
Improvements in diagnosis and treatment are also important.9,45 In the Czech Republic, for example, improved case-fatality from 1994 to 2009 had a substantial contribution to the reduction in the national CVD mortality rate.50 To achieve a greater impact, evidence-based treatments must be: available for all in need, cost-effective and achieve the recommended therapeutic targets. To be available for all in need, the first obstacle to be transposed is equal access to healthcare. Therefore, the importance of a structured national health systems has gained increasing attention, especially regarding the need for universal coverage, as payment for healthcare can enhance social disparities.51 Some initiatives have been successful in all world regions, as strengthening primary care and providing free-of-charge medication for chronic diseases.51 Evidence to suggest that paying for performance—instead of paying for services—improves healthcare is mixed and not yet conclusive, but it’s also a promising strategy. Health systems in HICs face the rising costs of technology intensive care for their aging populations and cost- effectiveness studies are essential to optimise allocation of resources.52,53 LMICs have a more difficult task, as they have to confront the double burden of diseases and the interaction between them, exemplified by the growing numbers of HIV-related CVDs.7,38 In these countries, health systems must be prepared for the rise of NCDs, but still cope with the burden of communicable and nutritional diseases, to which the social determinants are even more important, such as the housing conditions for rheumatic heart disease and Chagas heart disease. 11,54 In Africa, regional differences can be seen in the countries’ readiness to combat cardiovascular risk factors: 61% had funding available for NCD, however only 26% had a specific policy for diabetes.55 To achieve the recommended targets, health workers must be motivated and patients must be adherent, which is a challenge even to structured health systems, such as in the UK, where the majority of patients with IHD or those at high risk of developing CVD do not achieve lifestyle, risk factor and therapeutic targets suggested by the national prevention guidelines.56,57 Strategies such as the use of telephone calls to monitor adherence are good alternatives to be used.58 Another contribution of technology to Global Health is the spreading of information, which may contribute to the implementation of evidence-based interventions worldwide. However, while information travels even to remote areas, the uneven distribution of workforce is still a problem.59 Sub-Saharan Africa, for example, carries 24% of global disease burden, but has only 3% of health workforce.40 The poorer and rural areas of the globe have less health workers per 1000 inhabitants, mainly a consequence of poor infrastructure and train- ing.59 To counteract this trend, technology can also be used for training by online courses and monitoring at a distance, giving the opportunities for shared medical decision. The use of telemedicine for the interpretation of ECGs as a support for primary health in remote areas is a successful example that can be replicated in diverse areas.60 In a broader aspect, cooperation is essential if the global community wants to respond to conditions that affect their health. Regarding environmental sustainability, coordinated actions are important to achieve goals such as the reduction of pollution and, consequently climate changes.23,26 Global Health initiatives should focus on long-term strategies that promote peace, mitigate the impacts of poverty and are in synergy with the needs of the global and local communities.61 Global commitments to achieve reduction in NCD mortality, such as proposed by the United Nations that aims at a 25% reduction in premature NCD mortality by 2025 (the 25×25 goal) need efforts from local governments and international institutions.62 Research and technology development still needs to give more attention to neglected conditions. Diseases that mainly affect LMICs must be in the focus of research institutes worldwide and also be an opportunity for collaboration between countries. Good quality data about demography, epidemiology and the burden of diseases in this group of countries are also lacking, making identification of weaknesses, planning and implementation of solutions harder in these countries. Surveillance and information sharing is key to make the globe healthier.62
CONCLUSION
The approach to improve Global Health requires the development and implementation of solutions based on information derived from a variety of disciplines including medicine, demography, epidemiology, public health and economy to help policy decision making.4 Heart manuscripts have advanced significantly in these topics in the past 2 years, contributing to their understanding and dissemination. However, some particular gaps such as health education and effectiveness of screening programmes still need to be addressed in scientific literature. Trying to benefit from lessons learned across the world and adapting them to local appropriateness, the main objective of Global Health is to emphasise health equity. This task will be achieved by embracing promotion and prevention using population-wide interventions and also through effective delivery of clinical care at the individual level. Governments, foundations and the civil society from countries with different incomes must be willing to share responsibilities and funding in a common perspective, to reach health and well-being of people around the world.
Contributors: All authors participated actively in this study. All of them have seen and approved the submitted manuscript, which reports unpublished work not under consideration elsewhere. BRN, LCCB and DNM have done the literature review, article selection and designed the scope of the article. All authors contributed in the writing of the manuscript. BRN, LCCB and ALPR reviewed the final version.
Competing interests: None.
Provenance and peer review: Commissioned; externally peer reviewed.
References
1. Brown TM, Cueto M, Fee E. The World Health Organization and the transition from “international” to “global” public health. Am J Public Health 2006;96:62–72.
2. Koplan JP, Bond TC, Merson MH, et al. Towards a common definition of global health. Lancet 2009;373:1993–5.
3. Macfarlane SB, Jacobs M, Kaaya EE. In the name of global health: trends in academic institutions. J Public Health Policy 2008;29:383–401.
4. Global Health Education Consortium. Global vs international. 2009. http://globalhealthedu.org/Pages/GlobalvsInt.aspx
5. Institute of Medicine. The future of public health. Washington, DC: National Academy Press, 1988.
6. Hunter DJ, Reddy KS. Noncommunicable diseases. N Engl J Med 2013;369:1336–43.
7. Yusuf S, Reddy S, Ounpuu S, et al. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 2001;104:2746–53.
8. Cooney MT, Vartiainen E, Laatikainen T, et al. Cardiovascular risk age: concepts and practicalities. Heart 2012;98:941–6.
9. O’Flaherty M, Buchan I, Capewell S. Contributions of treatment and lifestyle to declining CVD mortality: why have CVD mortality rates declined so much since the 1960s? Heart 2013;99:159–62.
10. Baena CP, Chowdhury R, Schio NA, et al. Ischaemic heart disease deaths in Brazil: current trends, regional disparities and future projections. Heart 2013;99:1359–64.
11. Ntsekhe M, Damasceno A. Recent advances in the epidemiology, outcome, and prevention of myocardial infarction and stroke in sub-Saharan Africa. Heart 2013;99:1230–5.
12. de Fatima Marinho de Souza M, Gawryszewski VP, Ordunez P, et al. Cardiovascular disease mortality in the Americas: current trends and disparities. Heart 2012;98:1207–12.
13. Salomaa V, Havulinna AS, Koukkunen H, et al. Aging of the population may not lead to an increase in the numbers of acute coronary events: a community surveillance study and modelled forecast of the future. Heart 2013;99:954–9.
14. Jennings SM, Bennett K, Lonergan M, et al. Trends in hospitalisation for acute myocardial infarction in Ireland, 1997–2008. Heart 2012;98:1285–9.
15. Nedkoff L, Briffa TG, Knuiman M, et al. Temporal trends in the incidence and recurrence of hospitalised atherothrombotic disease in an Australian population, 2000–07: data linkage study. Heart 2012;98: 1449–56.
16. Sekikawa A, Miura K, Lee S, et al. Long chain n-3 polyunsaturated fatty acids and incidence rate of coronary artery calcification in Japanese men in Japan and white men in the USA: population based prospective cohort study. Heart 2014;100:569–73.
17. Rix TA, Joensen AM, Riahi S, et al. Marine n-3 fatty acids in adipose tissue and development of atrial fibrillation: a Danish cohort study. Heart 2013;99:1519–24.
18. Grandi NC, Brenner H, Hahmann H, et al. Calcium, phosphate and the risk of cardiovascular events and all-cause mortality in a population with stable coronary heart disease. Heart 2012;98:926–33.
19. Li K, Kaaks R, Linseisen J, et al. Associations of dietary calcium intake and calcium supplementation with myocardial infarction and stroke risk and overall cardiovascular mortality in the Heidelberg cohort of the European Prospective Investigation into Cancer and Nutrition study (EPIC-Heidelberg). Heart 2012;98:920–5.
20. de Brito-Ashurst I, Perry L, Sanders TA, et al. The role of salt intake and salt sensitivity in the management of hypertension in South Asian people with chronic kidney disease: a randomised controlled trial. Heart 2013;99:1256–60.
21. Islami F, Pourshams A, Vedanthan R, et al. Smoking water-pipe, chewing nass and prevalence of heart disease: a cross-sectional analysis of baseline data from the Golestan Cohort Study, Iran. Heart 2013; 99:272–8.
22. Hopstock LA, Fors AS, Bonaa KH, et al. The effect of daily weather conditions on myocardial infarction incidence in a subarctic population: the Tromso Study 1974–2004. J Epidemiol Community Health 2012;66:815–20.
23. Guo Y, Li S, Zhang Y, et al. Extremely cold and hot temperatures increase the risk of ischaemic heart disease mortality: epidemiological evidence from China. Heart 2013;99:195–203.
24. Puett RC, Hart JE, Yanosky JD, et al. Chronic fine and coarse particulate exposure, mortality, and coronary heart disease in the Nurses’ Health Study. Environ Health Perspect 2009;117:1697–701.
25. Miller KA, Siscovick DS, Sheppard L, et al. Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med 2007;356:447–58.
26. Pieters N, Plusquin M, Cox B, et al. An epidemiological appraisal of the association between heart rate variability and particulate air pollution: a meta-analysis. Heart 2012;98:1127–35.
27. Painschab MS, Davila-Roman VG, Gilman RH, et al. Chronic exposure to biomass fuel is associated with increased carotid artery intimamedia thickness and a higher prevalence of atherosclerotic plaque. Heart 2013;99:984–91.
28. Baker J, Mitchell R, Lawson K, et al. Ethnic differences in the costeffectiveness of targeted and mass screening for high cardiovascular risk in the UK: cross-sectional study. Heart 2013;99:1766–71.
29. Mundkur LA, Shivanandan H, Hebbagudi S, et al. Human cytomegalovirus neutralising antibodies and increased risk of coronary artery disease in Indian population. Heart 2012;98:982–7.
30. Zaman MJ, Bhopal RS. New answers to three questions on the epidemic of coronary mortality in south Asians: incidence or case fatality? Biology or environment? Will the next generation be affected? Heart 2013;99:154–8.
31. Zaman MJ, Philipson P, Chen R, et al. South Asians and coronary disease: is there discordance between effects on incidence and prognosis? Heart 2013;99:729–36.
32. Mathur R, Pollara E, Hull S, et al. Ethnicity and stroke risk in patients with atrial fibrillation. Heart 2013;99:1087–92.
33. Quan H, Chen G, Walker RL, et al. Incidence, cardiovascular complications and mortality of hypertension by sex and ethnicity. Heart 2013;99:715–21.
34. Sebastianski M, Makowsky MJ, Dorgan M, et al. Paradoxically lower prevalence of peripheral arterial disease in South Asians: a systematic review and meta-analysis. Heart 2014;100:100–5.
35. Tillin T, Hughes AD, Whincup P, et al. Ethnicity and prediction of cardiovascular disease: performance of QRISK2 and Framingham scores in a U.K. tri-ethnic prospective cohort study (SABRE—Southall And Brent REvisited). Heart 2014;100:60–7.
36. Sliwa K, Wilkinson D, Hansen C, et al. Spectrum of heart disease and risk factors in a black urban population in South Africa (the Heart of Soweto Study): a cohort study. Lancet 2008;371:915–22.
37. Syed FF, Ntsekhe M, Gumedze F, et al. Myopericarditis in tuberculous pericardial effusion: prevalence, predictors and outcome. Heart 2014;100:135–9.
38. Syed FF, Sani MU. Recent advances in HIV-associated cardiovascular diseases in Africa. Heart 2013;99:1146–53.
39. Mocumbi AO, Falase AO. Recent advances in the epidemiology, diagnosis and treatment of endomyocardial fibrosis in Africa. Heart 2013;99:1481–7.
40 Sliwa K, Mayosi BM. Recent advances in the epidemiology, pathogenesis and prognosis of acute heart failure and cardiomyopathy in Africa. Heart 2013;99:1317–22.
41. Makubi A, Hage C, Lwakatare J, et al. Contemporary aetiology, clinical characteristics and prognosis of adults with heart failure observed in a tertiary hospital in Tanzania: the prospective Tanzania Heart Failure (TaHeF) study. Heart 2014;100:1235–41.
42. Ogah OS, Rayner BL. Recent advances in hypertension in sub-Saharan Africa. Heart 2013;99:1390–7.
43. Blauwet LA, Libhaber E, Forster O, et al. Predictors of outcome in 176 South African patients with peripartum cardiomyopathy. Heart 2013;99:308–13.
44. Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation 2014;129: e28–e292.
45. Labarthe DR, Dunbar SB. Global cardiovascular health promotion and disease prevention: 2011 and beyond. Circulation 2012;125:2667–76.
46. Centers for Disease Control and Prevention. Global Health. Centers for Disease Control and Prevention, 2014.
47. Glantz S, Gonzalez M. Effective tobacco control is key to rapid progress in reduction of non-communicable diseases. Lancet 2012;379:1269–71.
48. de Korte-de Boer D, Kotz D, Viechtbauer W, et al. Effect of smokefree legislation on the incidence of sudden circulatory arrest in the Netherlands. Heart 2012;98:995–9.
49. Levy D, de Almeida LM, Szklo A. The Brazil SimSmoke policy simulation model: the effect of strong tobacco control policies on smoking prevalence and smoking- attributable deaths in a middle income nation. PLoS Med 2012;9:e1001336.
50. Davidkovova H, Kysely J, Kriz B, et al. Trends in cardiovascular mortality and hospitalisations, and potential contribution of inhospital casefatality rates to changes in national mortality in the Czech Republic 1994–2009. Heart 2013;99:409–16.
51. Mills A. Health care systems in low- and middle-income countries. N Engl J Med 2014;370:552–7.
52. Boriani G, Diemberger I, Biffi M, et al. Cost-effectiveness of cardiac resynchronisation therapy. Heart 2012;98:1828–36.
53. Gada H, Whitlow PL, Marwick TH. Establishing the cost-effectiveness of percutaneous coronary intervention for chronic total occlusion in stable angina: a decision-analytic model. Heart 2012;98:1790–7.
54. Nunes MC, Dones W, Morillo CA, et al. Chagas disease: an overview of clinical and epidemiological aspects. J Am Coll Cardiol 2013; 62:767–76.
55. Kengne AP, Sobngwi E, Echouffo-Tcheugui JB, et al. New insights on diabetes mellitus and obesity in Africa-Part 2: prevention, screening and economic burden. Heart 2013;99:1072–7.
56. Kotseva K, Jennings CS, Turner EL, et al. ASPIRE-2-PREVENT: a survey of lifestyle, risk factor management and cardioprotective medication in patients with coronary heart disease and people at high risk of developing cardiovascular disease in the UK. Heart 2012;98:865–71.
57. British Cardiac Society; British Hypertension Society; Diabetes UK; HEART UK; Primary Care Cardiovascular Society; Stroke Association. JBS 2: Joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practice. Heart 2005;91(Suppl 5):v1–52.
58. Rinfret S, Rodes-Cabau J, Bagur R, et al. Telephone contact to improve adherence to dual antiplatelet therapy after drug-eluting stent implantation. Heart 2013;99:562–9.
59. Crisp N, Chen L. Global supply of health professionals. N Engl J Med 2014;370:2247–8.
60. Alkmim MB, Figueira RM, Marcolino MS, et al. Improving patient access to specialized health care: the Telehealth Network of Minas Gerais, Brazil. Bull World Health Organ 2012;90:373–8.
61. Frenk J, Gomez-Dantes O, Moon S. From sovereignty to solidarity: a renewed concept of global health for an era of complex interdependence. Lancet 2014;383:94–7.
62. Bonita R, Magnusson R, Bovet P, et al. Country actions to meet UN commitments on non-communicable diseases: a stepwise approach. Lancet 2013;381:575–84.
 This work is licensed under a
This work is licensed under a