Laurențiu Pascalau2, Mihaela Valcovici1,2, Vladiana Turi1,2, Simona Drăgan1,2
1 “Victor Babes” University of Medicine and Pharmacy, Timisoara
2 Institute of Cardiovascular Diseases, Timisoara
BACKGROUND
Acute myocardial infarction (MI) mainly occurs in patients over 45 years old, but young adults can also suffer a MI. Causes of MI in young adults usually include: 1. atheromatous coronary artery disease (CAD); 2. non-atheromatous CAD; 3. hyper-coagulable states; 4. substance abuse (1). Although the incidence of MI among young people is not common, its consequences are significant, due to high morbidity, psychological effects and financial costs. Atheromatous CAD is linked to conventional risk factors in adults. In the study of Zimmermann et al, smoking was the most common risk factor (92%) in young adults (2). Th e cut-off age of 45 years old has been used in most of the studies to differenciate CHD or MI in young patients. Children born to parents with premature CHD have a tendency to higher incidence for lipid abnormalities, insulin resistance and obesity, a fact that can be linked to genetic inheritance (3). According to US data, about 80% of young subjects with MI are overweight or obese and at least one of the cardiovascular risk factors is the most important trigger in 96% of cases (4). Novel risk factors such as increased lipoprotein (a) and hyperhomocysteinaemia have recently been shown to have the same effects as conventional risk factors in younger people (5,6). Many epidemiological studies and reports have established hyperhomocysteinaemia as an independent risk factor for cardiovascular disease, cerebrovascular disease, dementia-type disorders and osteoporosisassociated fractures. Although combined folic acid and B-vitamin therapy has been shown to lower the levels of homocysteine, the controversial results of clinical trials have discarded the monitoring of these patients for risk follow-up (7). Unexplored areas such as psycho-social stress, anger, anxiety and the burn-out syndrome can accelerate coronary artery calcification and occurrence of MI in young adults (8). Among non-atheromatous causes of CAD, congenital coronary artery anomalies can manifest as MI in young adults. These cases are rare and come as a surprise in the cath-lab. Myocardial bridging, especially during systole, can also lead to MI9. Dissection in coronary arteries can suddenly happen in young adults, the left anterior descending artery being the culprit artery in most of the cases. Treatment by stenting or surgery represents the successful approach in all of the mentioned situations (10). Another cause of MI in young patients may be represented by septic emboli from vegetations occurring in aortic valve endocarditis, paradoxical emboli or emboli originating from coronary artery aneurysms (11). Hypercoagulable states, which occur in the antiphospholipid syndrome (APL), the nephrotic syndrome, factor V Leiden mutations or the use of contraceptive pills, are a developing cause of MI in young patients. APL syndrome implies recurrent arterial and venous thrombosis; it can be associated with other autoimmune diseases. The patients have premature atherosclerosis and increased platelet adhesivity. The level of antiphospholipid antibodies is closely linked to disease activity and a careful evaluation is required for diagnosis (12,13). Another cause of MI in young patients is related to the use of recreational drugs, the most frequently incriminated substance being cocaine, in about 48% of cases. A conventional risk factor added to substance abuse is smoking, leading to an exponential increase of MI risk occurrence (14). We present the case of a 27 years old male, physically fit without prior cardiovascular history, with acute myocardial infarction and thrombophilia.
CASE PRESENTATION
A 27 years old male patient was admitted to our clinic 12 hours after onset of a constrictive chest pain spreading to the interscapular-vertebral space and left upper limb and dyspnoea. Family history was positive for hypertension on the maternal side; the mother also suffered 6 spontaneous abortions in her lifetime; the father was not aware of any heart disease. No brothers or sisters. Conventional cardiovascular risk factors included dyslipidaemia (total cholesterol = 215 mg%, triglycerides = 225 mg%), obesity (body weight= 145 kg, H = 180 cm, BMI = 44.75kg/m2) and cigarette smoking (one pack/day for the last 10 years). The cardiovascular clinical examination revealed: blood pressure = 130/80 mmHg, heart rate 120 b/min, rhythmic heart sounds, late inspiratory rales over posterior bases in both lungs, symmetrical peripheral pulse present bilaterally. On the ECG sinus rhythm, Q wave in V1-V4, ST segment elevation of 3-4 mm in V2-V6 and 1-2 mm in DI, AVL were present (Figure 1).
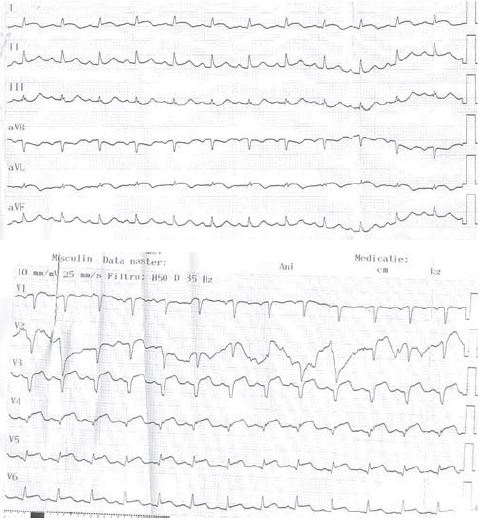
Figure 1. ECG on admission: sinus rhythm, Q wave in V1-V4, ST segment elevation of 3-4 mm in V2-V6 and 1-2 mm in DI, aVL.
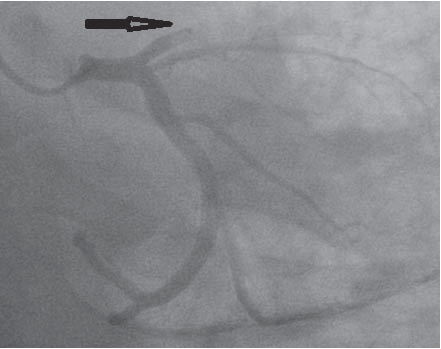
Figure 2. Coronary angiogram: thrombotic occlusion of the proximal left anterior descending (LAD) coronary artery.
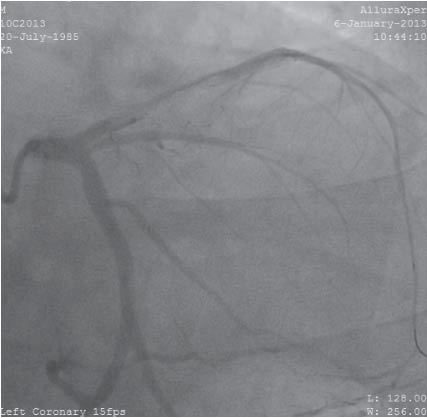
Figure 3. The aspect of the artery aft er multiple passes of thrombus aspiration and 250 mcg intracoronary nytroglicerine.
The echocardiographic examination revealed a normal-sized left ventricle with significant changes in kinetics, no movement in the apical half of the interventricular septum and in the apical third of the inferior and anterior wall, hypokinetic basal interventricular septum, EF = 40%, mild ischemic mitral regurgitation, dilated left atrium, mild pulmonary hypertension, and no pericardial effusion. Laboratory findings on admission revealed increased enzymes of myocardial necrosis (CPK = 2288 U/l, CPK-MB = 227 U/l). The diagnosis was acute anterior ST-elevation myocardial infarction (STEMI). The patient underwent an emergency coronary angiography that pointed out a thrombotic occlusion of the proximal left anterior descending (LAD) coronary artery (Figure 2), without the visualization of the distal territory. Export catheter was used and thrombus aspiration was performed. Multiple passes of thrombus aspiration were performed.
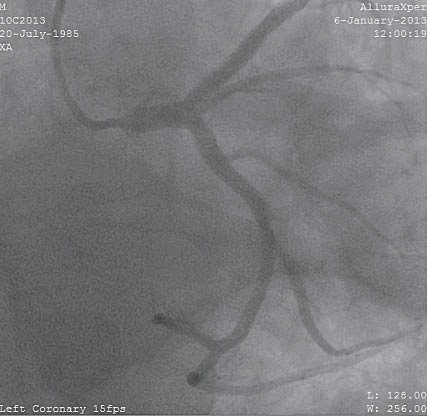
Figure 4. Caudal left -anterior-oblique view – final result after stenting.
Figure 5. Cranial right-anterior-oblique view – final result after stenting.
Afterwards, intracoronary eptifibatide in a dose of 2 mcg/kg and 250 mcg of nitro-glycerine were given. A 90% atherosclerotic stenosis was detected in with a remaining thrombus inside the LAD (Figure 3). The next step was stenting of the culprit artery – proximal LAD with the seizing of the remaining thrombus between the stent and the vessel wall. Approximately one minute aft er stenting, 500 mcg verapamil were given intracoronary through the guide catheter. The final result was good, without any remaining stenosis, no dissection proximally or distally, TIMI III and myocardial blush stage 3 (Figure 4 and Figure 5). Massive thrombosis in the LAD occurring at a young age required further investigation of causes responsible for hypercoagulable states (C and S proteins, Factor II – G20210A, Factor V Leiden, polymorphism of the human methylenetetrahydrofolate reductase gene, antithrombin III, homocysteine, lupus anticoagulant). The screening for thrombophilia, performed on the fourth day after stenting, revealed an increased homocysteine level = 19,12 um/l (NV – A1298C, low levels of antithrombin III (78.5%, with NV of 79,4-112) and normal values for protein C and S. Th e lupus anticoagulant was absent. Factor II, Factor V and methylenetetrahydrofolate reductase gene – C677T mutations were absent. The screening for thrombophilia was made 48h aft er the last dose of heparin. Due to presence of thrombophilia, dual antiplatelet therapy was associated with oral anticoagulant treatment. Evolution under therapy was very good, with a significant decrease of myocardial necrosis enzymes after three days. The patient was discharged after eight days with dual antiplatelet and oral anticoagulant therapy, a betablocker, diuretic and a statin. The treatment was well tolerated and no ischemic recurrence was detected.
DISCUSSIONS
Atherosclerotic disease is a generalized disorder of the vascular system characterized by long-term atheromatous plaque formation developing in athero-thrombotic obstructive lesions that leads to tissue damage (15). Angina and acute myocardial infarction (MI) are the clinical manifestations of the chronic development of coronary artery atheroma. The underlying processes that lead to atheroma formation and coronary thrombosis are complex, involving imbalance of various systems that regulate vasoactivity, adhesion molecules, inrombophiflammation, lipid metabolism, coagulation and fi brinolysis (15). The pathogenesis of arterial thrombotic disease involves multiple genetic and environmental factors related to atherosclerosis and thrombosis. The generally accepted conventional risk factors include smoking, hypertension, hyperlipidaemia, obesity, diabetes and a positive family history (15,16). Acute coronary syndrome is rarely encountered in young adults and may have unusual causes. Atherosclerotic plaque is not always present and non-atherosclerotic causes of coronary artery disease such as thrombophilia should be considered especially in young patients with myocardial infarction. Thrombophilia can be defined as a hereditary or acquired increased risk of thrombosis. The hereditary causes of thrombophilia are defi ciencies of protein C, protein S and antithrombin III, factor V Leiden, hyperhomocysteinaemia, prothrombin G20210A polymorphism and elevated levels of factor VIII, von Willebrand factor (vWF) and fi brinogen levels. The acquired causes are antiphospholipid antibodies, cancer and hyperhomocysteinaemia due to mild nutritional folic acid, vitamin B12 or B6 deficiencies or associated hyperlipidaemia. Acquired thrombophilia can also occur in persistent inflammatory conditions and myelo-proliferative disorders (17). The clinical manifestations of thrombophilia are venous thromboembolism at a young age, thrombosis at different sites (cerebral sinuses, portal), recurrent foetal loss, pre-eclampsia, premature atherosclerosis, and myocardial infarction at a young age without any conventional risk factors and family history of venous thromboembolism (17). The main event in the pathogenesis of any thrombotic event is the perturbation of haemostasis17. This perturbation may be genetically determined (Figure 6).
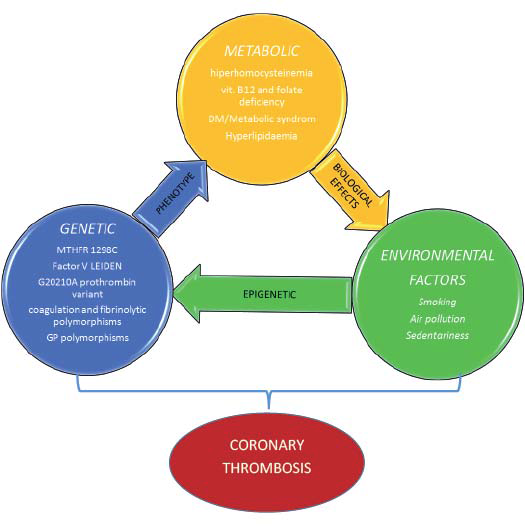
Figure 6. Interplay of genetic, metabolic and environmental factors in inherited hypercoagulable states.
But, since the onset of thrombosis in the majority of cases is at a later stage, it is unlikely that genetic causes may be the sole determinant. This points towards a gene-environment interaction in thrombosis. There are certain distinctions between arterial and venous thrombosis. The thrombus is platelet rich in arterial thrombosis and fibrin rich in venous thrombosis. Additionally in arterial thrombosis, there is presence of atheroma which represents vascular wall damage (15). In the particular case of our patient, multiple conventional cardiovascular risk factors were present such as: sex, dyslipidaemia, obesity and smoking. Still, these factors cannot explain the occurrence of MI at such a young age and the massive thrombosis in the LAD. After multiple passes of thrombus aspiration in the proximal and medium segments of LAD and retrieval of a large quantity of thrombus, a long 90% stenosis was noticeable along with a massive remaining thrombus in the proximal segment of LAD (Figure 3). The remaining thrombus in the coronary artery could not be retrieved even aft er intracoronary ebtifi batide administration. Afterwards, stenting of the lesion in the culprit artery was performed (prolonged inflation of 45 seconds), with seizing of the remaining thrombus between the stent wall and the vessel wall. One minute after stenting, although in the absence of any no-reflow phenomenon, 500 cmg verapamil were given intracoronary through the guide catheter. Verapamil is a calcium channel blocker that improves relaxation in the vascular wall and increases myocardial perfusion through the blockage of calcium in the calcium channel in the coronary arteries (18). Intracoronary verapamil administration can prevent negative ventricular remodelling and can improve left ventricular function due to microvascular dysfunction recovery. The mechanism of action of verapamil is decrease of microcirculation spasm and by improvement of myocardial blood flow in patients with AMI. The suspicion of thrombophilia has arisen due to massive thrombosis in LAD and to a history of 6 spontaneous abortions on the maternal side. The evaluation of the patient included, on the fourth day after onset of symptoms, detection of thrombophilia markers that revealed hyperhomocysteinaemia, heterozygote mutation of the human methylenetetrahydrofolate reductase gene and low levels of antithrombin III. Evaluation of thrombophilia markers in the mother was declined. Because the patient had thrombophilia and massive thrombus in the LAD, at discharge, we opted for indefinite anticoagulant therapy associated in the first 6 months with dual antiplatelet therapy (clopidogrel + acetylsalicylic acid), and aft er six months, with just one antiplatelet drug (acetyl salicylic acid). At discharge, we did not prescribe any homocysteine lowering drugs (folic acid, vitamins B6 and B12) because the clinical trials in this area were negative for reducing the risk for cardiovascular events aft er AMI. On the contrary, they can exert a harmful action, one of the reasons why they are not generally recommended (20).
CONCLUSIONS
Inherited thrombophilia is a genetic disorder predisposing to thrombosis which may manifest occasionally, usually in the presence of trigger factors. Th rombophifllia induces a hypercoagulable state, which, together with other cardiovascular risk factors, may explain the arterial thrombosis in this young patient. It is very important to early diagnose these genetic disorders, because they influence long-term treatment and outcomes. Due to poor long-term prognosis, it is vital to diagnose this condition before a thrombotic event. This is difficult to achieve, because the evaluation expenses are high and they must be covered by the patient. In the case of our patient, the fact that the mother had six miscarriages before, should have led to the suspicion of thrombophilia as cause for the spontaneous abortions. Early diagnosis could have changed the outcomes in this patient. In practice, this condition is responsible for a small percentage of acute myocardial infarctions, in patients who are mostly young, and the prognosis is poor. Usually, in the absence of a proper diagnosis, these patients do not receive adequate treatment.
Conflict of interest: none declared.
References
1. M Egred, G Viswanathan, G K Davis – Myocardial infarction in young adults, Postgrade Med. J. 2005; 81 (962): 741-5.
2. Angiographic characteristics, risk factors and prognosis, coronary artery surgery study register (CASS). J Am Coll Cardiol 1995; 26:654.
3. Berenson GS, Srinivasan SR, Bao W, et al. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults: the Bogalusa heart study. N Engl J Med 1998; 338: 1650-6.
4. Zarich S, Luciano C, Hulford J, Abullah A: Prevalence of metabolic syndrome in young patients with acute MI: does the Framingham Risk Score underestimate cardiovascular risk in this population? Diab Vasc Dis Res 2006; 3:103-107.
5. Foody JM, Milberg JA, Robinson K, et al. Homocysteine and lipoprotein (a) interact to increase coronary artery disease risk in young men and women. Atherosclerosis Th rom Vasc Biol 2000; 20: 493-9.
6. Issar HS, Puri VK, Narain VS, et al. Lipoprotein (a) and lipid levels in young patients with myocardial infarction and in their first degree relatives. Indian Heart J 2001; 53:463-6.
7. Bradley A, Maron M.D. and Joseph Loscalzo, M.D., Ph.D., The treatment of hyperhomocysteinaemia. Annu Rev Med. 2009; 60:39-54.
8. Iribarren C, Sydney S, Bild DE, et al. Association of hostility with coronary artery calcification in young adults; the CARDIA study. Coronary artery risk determinants in young adults. JAMA 2000; 283:2526-51.
9. Mahlenkamp S, hort W, Ge J, et al. Update on myocardial bridging. Circulation 2006; 106:2616.
10. Butler R, Webster MWI, Davies GK, et al. Spontaneous dissection of native arteries. Heart 2005; 91:223-4.
11. Mathew J, Addai T, Anand A. Clinical features, site of involvement, bacteriological fi ndings and outcomes of infective endocarditis in intravenous drug users. Arch Intern Med 1995; 155:1641-6.
12. Tanis BC, Bloemankamp DG, Van Den Bosch MA, et al. Prothrombotic coagulation defects and cardiovascular risk factors in young women with acute myocardial infarction. Br J Haematol 2003; 1:471.
13. Petiti DB. Combination estrogen-progestin oral contraceptives. N Engl Med 2003; 349: 1443-50.
14. Hollander JE, Todd KH, Green G, et al. Chest pain associated with cocaine: an assessment of prevalence in suburban and urban emergency departments. Ann Emerg Med 1995; 26:671-6.
15. Ross R. Atherosclerosis – an infl ammatory disease. N Engl J Med 1999; 340:115-26.
16. Middeldorp S, Buller HR, Prins MH, Hirsh J. Approach to the thrombophilia patient. Hemostasis and Th rombosis. Basic Principles and Clinical Research, Lippincott Williams and Wilkins 2000; 4: 1085-1100.
17. Enas EA. Dhawan J, Petkar S. Coronary artery disease in Asian Indians: lessons learnt and the role of lipoprotein (a). Indian Heart J 1997; 49: 25-34.
18. Dong-bao L, Qi H, Zhi L, Shan W, Wei-ying J et al. Predictors and long-term prognosis of angiographic slow/no-refl ow phenomenon during emergency percutaneous coronary intervention for ST-elevated acute myocardial infarction. Clin Cardiol. 2010 ; 33(12):7-12.
19. Su Q, Li L, Liu Y. Short-term eff ect of verapamil on coronary no-reflow associated with percutaneous coronary intervention in patients with acute coronary syndrome: a systematic review and meta-analysis of randomized controlled trials. Clin Cardiol. 2013; 36(8):11-6.
20. Bønaa KH1, Njølstad I, Ueland PM, Schirmer H, Tverdal A, Steigen T, Wang H, Nordrehaug JE, Arnesen E, Rasmussen K; NORVIT Trial. Investigators Homocysteine lowering and cardiovascular events after acute myocardial infarction. N Engl J Med. 2006; 354(15):1578-88.
 This work is licensed under a
This work is licensed under a