Anda Ciobanu1, Radu Stavaru1, Oana Mirea1,2, Petre Ciobanu3, Ruxandra Deliu1, Octavian Istratoaie1,2, Ionut Donoiu1,2, Constantin Militaru1,2
1 Department of Cardiology, County Clinical Emergency Hospital, Craiova, Romania
2 Department of Cardiology, University of Medicine and Pharmacy, Craiova, Romania
3 Department of Cardiology, „Filantropia” Hospital, Craiova, Romania
Abstract: Prinzmetal’s angina is characterized by recurrent episodes of chest pain which occur during rest or sleep, asso-ciated with transient elevation of the ST segment on the electrocardiogram. The underlying mechanism is focal or diffuse coronary artery spasm that can affect one or multiple coronary artery sites simultaneously or consecutively. We report the case of a 53-year-old woman with persistent angina which presented with multivessel spasm recorded during coronary angiography without provocation test. The symptomatology of the patient was effectively relieved by combining two calcium channel blockers with a selective inhibitor of phosphodiesterase–3 and a long-lasting nitrate. Keywords: Prinzmetal angina, coronary artery spasm, treatment.
INTRODUCTION
Typical angina is characterized by recurrent attacks of chest pain, caused by exertion, and relieved by rest or by administration of nitroglycerin. In 1959, Myron Prinzmetal and his colleagues first described an atypi-cal form of angina, which they named ’variant angina’1. Chest pain in variant angina is not caused by physi-cal exercise, it almost always occurs at rest or during sleep, and it is usually associated with transient ST seg-ment elevation on the electrocardiogram. Even thou-gh it is uncommon, Prinzmetal’s angina has important implications for patient’s quality of life, morbidity and cardiac mortality, being associated with potentially lethal complications, such as ventricular tachycardia, ventricular fibrillation, advanced atrioventricular block and asystole2,3.
CASE PRESENTATION
A 53-year-old woman presented to the emergency de-partment for repeated episodes of constrictive chest pain with irradiation at the submandibular level, 2-3 minutes in duration, occurring during sleep, in case of emotional stress or small physical exertion. She had suffered from the anginal attacks for 4 years, but in the previous month, episodes increased in frequency and appeared during mild exertion, as well. Coronary angiography was performed three years prior, when a severe spasm of the right coronary artery was trigge-red by contrast injection (Figure 1, A–D). At that point, the patient was treated with Verapamil 240 mg/ day, Isosorbide dinitrate 20 mg bid, Atorvastatin 40 mg/day, Aspirin 100 mg/day, Trimetazidine 35 mg bid. Other clinical history included recent menopause and significant family history (brother died suddenly at age 45).
Clinical exam revealed an overweight patient (BMI 26.2 kg/m2), blood pressure was 140/80 mmHg, heart rate was 55 bpm, rhythmic heart sounds with no murmurs and no pulmonary rales.
The resting electrocardiogram (ECG) at presentation showed sinus rhythm, heart rate of 55 bpm, QRS axis 0°, negative T waves in infero-lateral leads (Figure 2).
On transthoracic echocardiography, left ventricular structure and systolic function were normal, with an ejection fraction of 65% calculated with the Simpson’s biplane method, and normal segmental contraction. Transmitral diastolic flow derived from Doppler echo-cardiography as well as the E/e’ ratio showed normal diastolic function of the left ventricle and normal filling pressures. No abnormal findings were reported during echocardiography.
Standard blood tests were within normal range, in-cluding the myocardial necrosis specific markers whi-ch were normal at admission and without any change during hospitalization.
Due to the unstable symptoms, the patient was hos-pitalized for further assessment and treatment. During hospitalization, the patient presented several episodes of severe chest pain, 2 to 3 minutes in duration, asso-ciated with ST segment elevation of up to 4 mm in leads DII, DIII, aVF, V5-V6, and ST segment downward depression in V1-V2 (Figure 3).
24-hour ECG monitoring revealed episodes of tran-sient ST segment elevation with a duration of up to 2 minutes without conduction or rhythm disturbances.
In this context, coronary angiography reevaluation was considered appropriate and revealed a 70% steno-sis in the first diagonal branch of left anterior descen-ding artery (Figure 4, A). Although the area supplied by the affected artery did not seem significant, it was decided to electively implant a stent in a programmed procedure. Within 72 hours, a second coronary an-giography was performed with the intent of percu-taneous coronary intervention (PCI), but it revealed normal fl ow in the first diagonal and severe spasm in the middle segment of left anterior descending artery, which was rapidly relieved after intracoronary nitro-glycerin administration (Figure 4, B–D). The second coronary angiography allowed us to conclude that coronary vasospasm with multiple localizations (right coronary artery, left anterior descendent artery, and diagonal branch) was the underlying mechanism for the clinical symptoms.
The persistence of angina episodes forced us to try uncommon therapeutic solutions: the association of two calcium channel blockers and Cilostazol. The pa-tient was treated with 360 mg of Diltiazem, 5 mg of Amlodipine, 40 mg of Isosorbide dinitrate, 200 mg of Cilostazol, 70 mg of Trimetazidine, 75 mg of Clopido-grel, 40 mg of Atorvastatin and 1000 mg of Magne-sium orotate. The angina episodes were not repeated during hospitalization. At the most recent follow-up visit, almost one year after the hospitalization, the pa-tient reported no recurrence of chest pain.
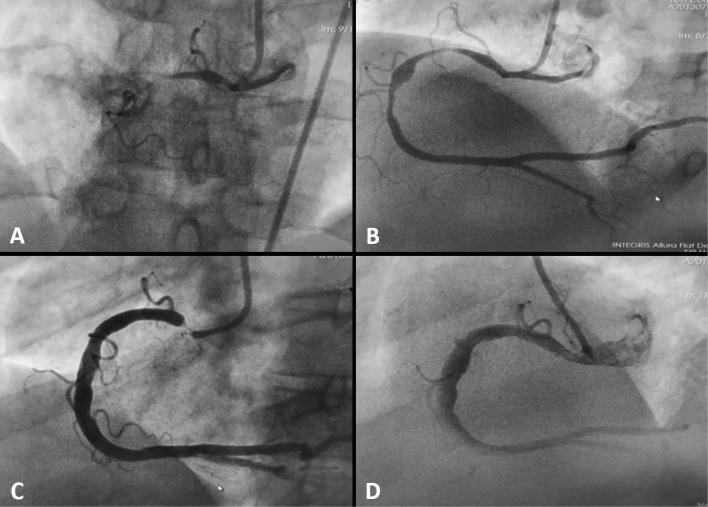
Figure 1. Coronary angiography from 2015. Severe right coronary artery spasm with complete occlusion (A); persistence of diffuse spasm predominant in the proximal and middle segments (B); severe focal spasm at the origin of right coronary artery (C); the vessel after almost complete remission of the spasm (D).
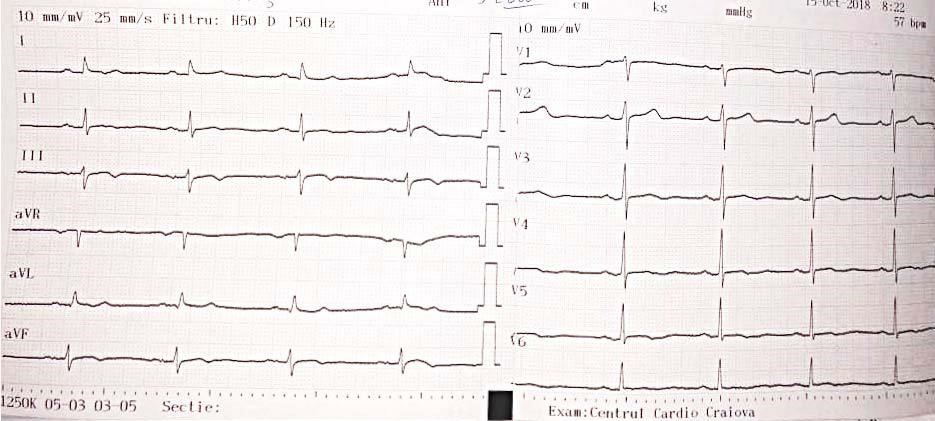
Figure 2. Resting electrocardiogram at presentation, without chest pain.
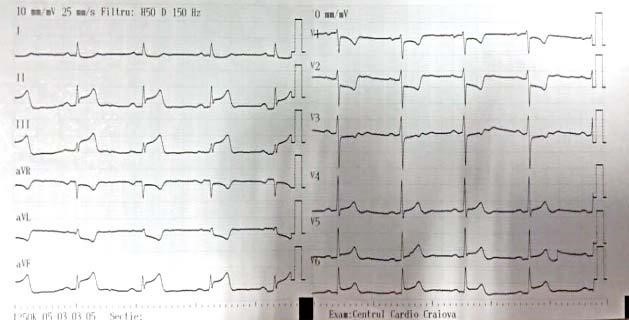
Figure 3. Electrocardiogram recorded during chest pain episode.
DISCUSSION
The case presented here raises some important issues which are worth discussing: (i) the occurrence of multivessel spasm in vasospastic angina recorded during coronary angiography without provocation; (ii) why a previously well-controlled patient became unstable; (iii)the medical options in patients with symptoms not controlled by single calcium channel blocker administration.
Vasospastic angina is a form of angina in which co-ronary artery spam is causing ischemia. Use of the term Prinzmetal’s angina (variant angina), should be restricted to cases in which there is transient ST seg-ment elevation during anginal episodes.
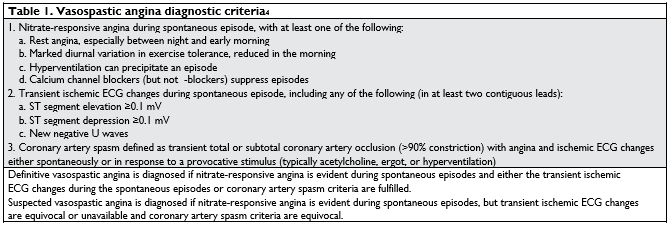
According to the Coronary Vasomotion Disorders In-ternational Study Group (COVADIS) the diagnosis of va-sospastic angina requires the fulfi llment of three types of criteria: classical clinical manifestations, transient ECG changes during chest pain episodes, angiographic demonstration of coronary artery spasm4 (Table 1).
Coronary artery spasm is the central mechanism of ischemia in Prinzmetal’s (variant) angina5,6. A tempo-rary increase in vascular tonus in a subepicardial co-ronary artery with or without atherosclerotic changes may temporarily cause critical hypoperfusion in a myo-cardial area, resulting in symptoms specific to variant angina and transient electrocardiographic abnormali-ties. The mechanism of coronary spasm is complex and involves multiple pathogenic pathways such as: endothelial dysfunction, smooth muscle cell hyperre-activity, infl ammation, decreased nitric oxide availability, oxidative stress, magnesium defi ciency, autonomic nervous system imbalance, genetic polymorphisms7,8.
Coronary artery spasm usually involves a major ar-tery or large branches, it can be focal or diffuse, it can affect one site or multiple sites of one artery, or more than one vessel at a time, and in some patients it has migratory character9,10. Multivessel spasm has variable prevalence, being reported in 9-52% of patients11,12 and it is one of the predictors of major adverse car-diac events, as part of the clinical risk score develo-ped by the Japanese Coronary Spasm Association13. In patients with variant angina, catheter stimulation of a coronary artery during angiography may precipitate spasm with angina and ST-segment elevation. Catheter-induced spasm is usually located in the proximal segment of the right coronary artery.
Prinzmetal’s angina can have a cyclical evolution, with long periods of calm followed by reappearance of angi-nal attacks. The exact cause of this is not known yet, but it could be related to the variability in the degree of local vascular hypersensitivity, or in the intensity of an unknown provoking stimulus14. The patient we presented had recently begun menopause. Lower le-vels of estradiol aggravate endothelial dysfunction and are associated with an increased frequency of angina attacks. Also, the premenopausal period determines variations in estrogen hormone levels which, accor-ding to the results of Kawano et al.15, induce changes in endothelial function and the cyclical appearance of myocardial ischemia in women with vasospastic angina depending on the period of menstrual cycle associated with the level the lowest estrogen hormone. In a study on 15 women estrogen supplementation suppressed the hyperventilation-induced attacks in women with variant angina, an effect which could be explained by an improvement of endothelial function16.
Nitrates and calcium channel blockers are the mai-nstay of treatment in vasospastic angina7. Long-acting calcium channel blockers are highly effective in re-ducing angina frequency and also improve long-term prognosis17. A combined use of two calcium channel blockers in patients with refractory symptoms has been proposed by some authors, but evidence about its effectiveness is scarce10. In a 1980 report by Kishi-da18 the use of Nifedipine and Diltiazem in 15 patients completely suppressed angina in 11 patients and de-creased the episodes by at least half in 4 patients. This approach has some pharmacological basis, as there are signifi cant differences in the mechanism of action between the three main types in the class19. In our patient we preferred to associate Amlodipine to Dilti-azem due to the low heart rate, as Verapamil is known to be more bradycardia inducing.
Short-acting nitrates are very effective in treating anginal attacks. For reducing the frequency of chest pain episodes in patients with vasospastic angina cur-rent guidelines recommend the use of long-acting nitrate agents in combination with calcium channel blockers in patients who remain symptomatic7.
Other agents have been tried with variable success, including endothelin antagonists20, Nicorandil, Fasudil (Rho-kinase inhibitor)7, Cilostazol21 or Magnesium22. The use of non-selective beta-blockers should be avoi-ded as they cause a blockade of vasodilatory effects on -adrenergic receptors, covering the effects of sym-pathetic stimulation in a pure -adrenergic vasocon-strictor response23. Also, high doses of Aspirin, which may decrease prostaglandin production and worsen coronary artery spasm, should be avoided24.
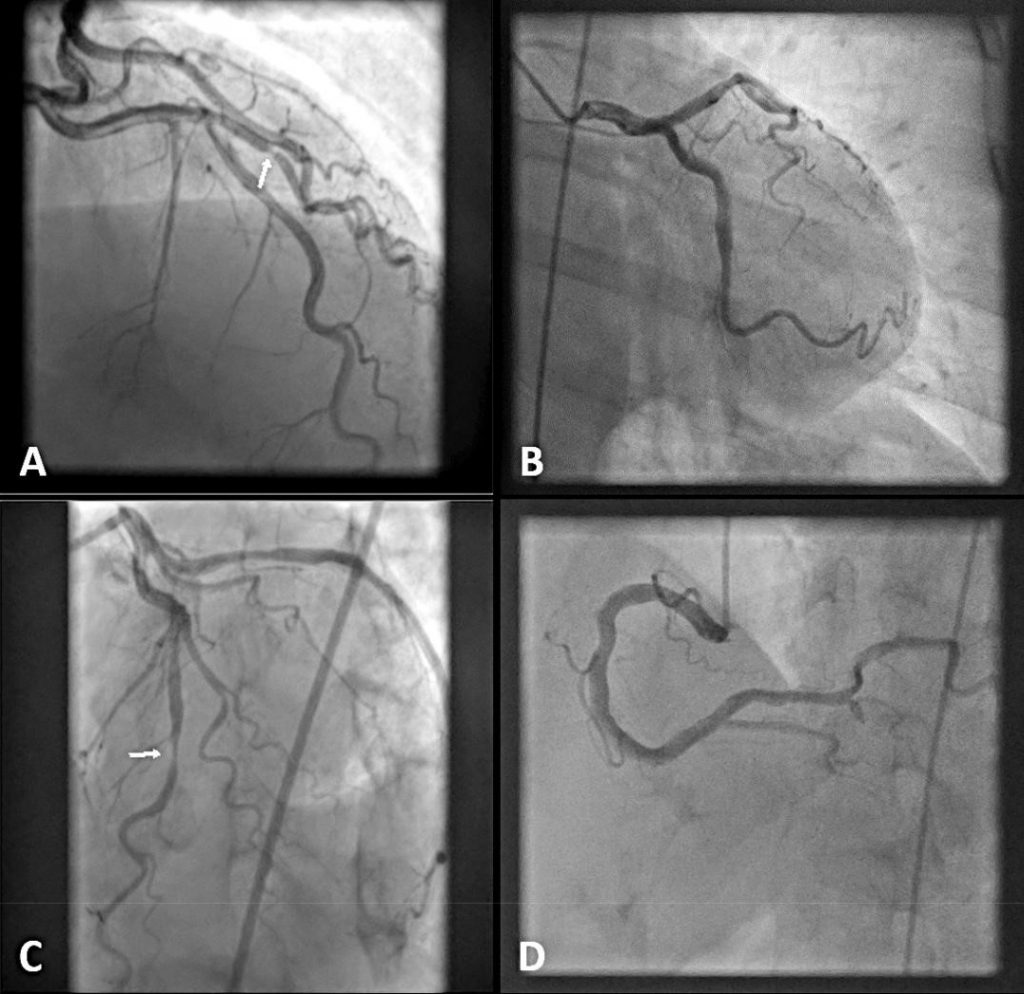
Figure 4. Coronary angiography from 2018. 70% stenosis of first diagonal branch of left anterior descending artery (A); left circumflex artery without significant lesions (B); diffuse spasm of left anterior descending artery with severe obstruction in middle segment and diffuse spasm of first diagonal branch but without focal obstruction (C); right coronary artery with diffuse atheroma plaques but no stenosis or spasm (D).
CONCLUSION
Coronary artery spasm in Prinzmetal’s angina may be extremely variable in terms of localization and appea-rance over time. In subjects with persistent episodes of chest pain despite conventional treatment, a combi-nation between two calcium channel blockers, a long-lasting nitrate and a selective inhibitor of phosphodies-terase–3 could be helpful to relieve symptoms.
Conflict of interest: none declared.
References
1. Prinzmetal M, Kennamer R, Merliss R, Wada T, Bor N. Angina pec-toris, I: a variant form of angina pectoris: preliminary report. Am J Med. 1959;27:375-88.
2. Unverdorben M, Haag M, Fuerste T, Weber H, Vallbracht C. Vaso-spasm in smooth coronary arteries as a cause of asystole and syn-cope. Cathet Cardiovasc Diagn. 1997;41(4):430-4.
3. Chin A, Casey M. Variant angina complicated by polymorphic ven-tricular tachycardia. Int J Cardiol. 2010;145(2):e47-e49.
4. Beltrame JF, Crea F, Kaski JC, Ogawa H, Ong P, Sechtem U, Shi-mokawa H, Bairey Merz CN; Coronary Vasomotion Disorders International Study Group (COVADIS). International standard-ization of diagnostic criteria for vasospastic angina. Eur Heart J. 2017;38(33):2565-8.
5. Olivia PB, Potts DE, Plus RG. Coronary arterial spasm in Prinzmetal angina. Documentation by coronary arteriography. N Engl J Med. 1973;283:745-51.
6. Dhurandhar RW, Watt DL, Silver MD, et al. Prinzmetal’s variant form of angina with arteriographic evidence of coronary arterial spasm. Am J Cardiol. 1972;30:902-5.
7. Picard F, Sayah N, Spagnoli V, Adjedj J, Varenne O. Vasospastic an-gina: A literature review of current evidence. Arch Cardiovasc Dis. 2018;pii:S1875-2136(18)30132-3.
8. MacAlpin RN. Some observations on and controversies about coro-nary arterial spasm. Int J Cardiol. 2015;181:389-98.
9. Ozaki Y, Keane D, Serruys PW. Fluctuation of spastic location in pa-tients with vasospastic angina: a quantitative angiographic study. J Am Coll Cardiol. 1995;26(7):1606-14.
10. Yasue H, Nakagawa H, Itoh T, Harada E, Mizuno Y. Coronary ar-tery spasm–clinical features, diagnosis, pathogenesis, and treatment. J Cardiol. 2008;51(1):2-17.
11. Kaski JC, Maseri A. Coronary artery spasm: European view. Coro-nary Artery Dis. 1990;1:660-7.
12. Yasue H, Kugiyama K. Coronary spasm: clinical features and patho-genesis. Intern Med. 1997;36(11):760-5.
13. Takagi Y, Takahashi J, Yasuda S, Miyata S, Tsunoda R, Ogata Y, Seki A, Sumiyoshi T, Matsui M, Goto T, Tanabe Y, Sueda S, Sato T, Oga-wa S, Kubo N, Momomura S, Ogawa H, Shimokawa H; Japanese Coronary Spasm Association. Prognostic stratification of patients with vasospastic angina: a comprehensive clinical risk score devel-oped by the Japanese Coronary Spasm Association. J Am Coll Car-diol. 2013.24;62(13):1144-53.
14. Bertrand ME, Simoons ML, Fox KA, Wallentin LC, Hamm CW, Mc-Fadden E, de Feyter PJ, Specchia G, Ruzyllo W. Management of acute coronary syndromes: acute coronary syndromes without persistent ST segment elevation; recommendations of the Task Force of the European Society of Cardiology. Eur Heart J. 2000;21(17):1406-32.
15. Kawano H, Motoyama T, Ohgushi M, Kugiyama K, Ogawa H, Yasue H. Menstrual cyclic variation of myocardial ischemia in premenopaus-al women with variant angina. Ann Intern Med. 2001;135(11):977-81.
16. Kawano H, Motoyama T, Hirai N, Kugiyama K, Ogawa H, Yasue H. Estradiol supplementation suppresses hyperventilation-induced at-tacks in postmenopausal women with variant angina. J Am Coll Car-diol. 2001;37:735-40.
17. Nishigaki K, Inoue Y, Yamanouchi Y, Fukumoto Y, Yasuda S, Sueda S, Urata H, Shimokawa H, Minatoguchi S. Prognostic effects of calcium channel blockers in patients with vasospastic angina–a meta-analysis. Circ J. 2010;74(9):1943-50.
18. Kishida H. Application of calcium antagonists in patients with Prinzmetal angina pectoris. In: Fleckenstein A, Rosskamm H, eds. Calcium Antagonismus. Berlin: Springer-Verlag; 1980:246-51.
19. Henry PD. Comparative pharmacology of calcium antagonists: Nife-dipine, verapamil and diltiazem. The American Journal of Cardiology. 1980;46(6):1047-58.
20. Krishnan U, Win W, Fisher M. First report of the successful use of bosentan in refractory vasospastic angina. Cardiology. 2010;116(1): 26-8.
21. Yoo SY, Song SG, Lee JH, Shin ES, Kim JS, Park YH, Kim J, Chun KJ, Kim JH. Efficacy of cilostazol on uncontrolled coronary vasospastic angina: a pilot study. Cardiovasc Ther. 2013;31(3):179-85.
22. Miyagi H, Yasue H, Okumura K, Ogawa H, Goto K, Oshima S. Ef-fect of magnesium on anginal attack induced by hyperventilation in patients with variant angina. Circulation. 1989;79:597-602.
23. Robertson RM, Wood AJJ, Vaughn WK, et al. Exacerbation of vaso-tonic angina pectoris by propranolol. Circulation 1982;65:281-5.
24. Miwa K, Kambara H, Kawai C. Effect of aspirin in large doses on at-tacks of variant angina. Am Heart J. 1983;105:351-5.
 This work is licensed under a
This work is licensed under a