Gabriela Puha1,2, Catalina Lionte1,2, Cristina Bologa1,2, Laurentiu Sorodoc1,2
1 2nd Internal Medicine Clinic, “Sf. Spiridon” Emergency Clinical County Hospital, Iasi, Romania
2 “Gr. T. Popa” University of Medicine and Pharmacy, Iasi, Romania
INTRODUCTION
The products collectively called “ethnobotanics” or “legal highs” contain chemicals or mixtures of chemicals with plant products often producing similar effects to those of high-risk drugs. A wide variety of such products can be purchased via the Internet or in stores for cigarettes and weedshops. Most of the time, the identification of the substances contained in these products is very difficult, because their concentration and composition are very varied and the consumers do not declare the trade name of the consumed psychoactive substance. Frequently, the ethnobotanics
contain synthetic cannabinoids, which do not appear in the urine drug screening1-3. The effects due to the consumption of these products, rolled into a cigarette, are multiple: altered perceptions, psychotic symptoms (extreme anxiety, confusion, paranoia, hallucinations), nausea, suicidal ideation, increases of blood pressure (BP) and heart rate (HR).
CASE REPORT
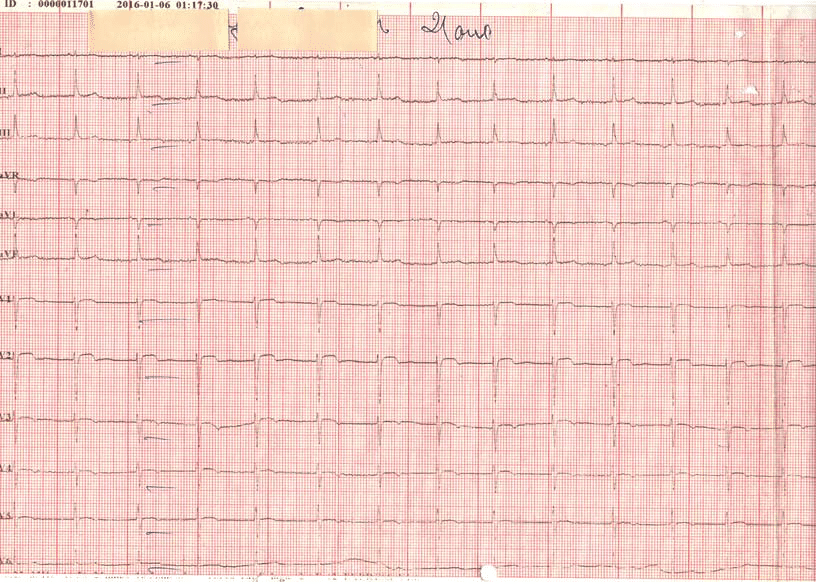
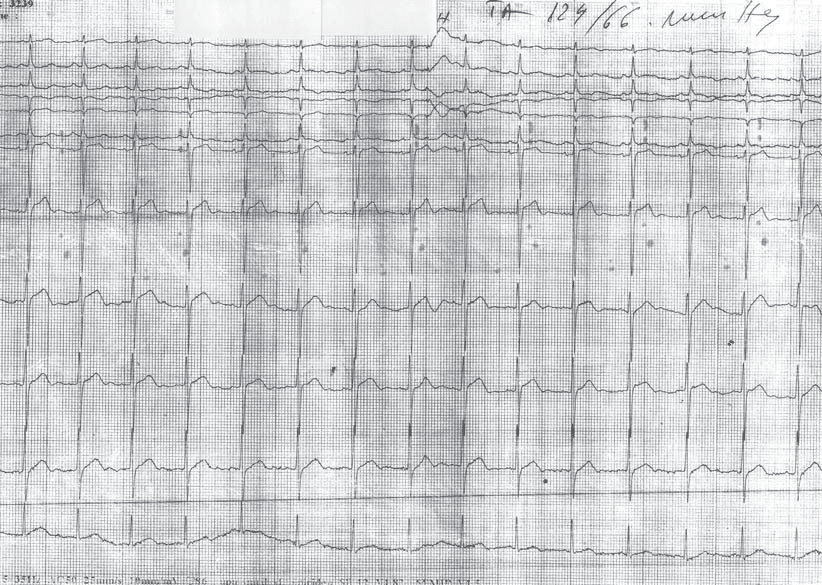
A 21 years old patient, smoker, without a known pathological personal history, comes in for fainting occurred after smoking of ethnobotanics, complaining of significant thoracic pain, ccompanied by shortness of breath before the syncope episode. The initial ECG in the Emergency Department (ED) – Figure 1, shows sinus rhythm (SR) 65/min, QRS axis +90 degrees, biphasic T +/- in DII, DIII, AVF, and 2 mm ST elevation in V1, V2 with negative T waves in V3-V5. On the admission in the clinic he had a normal clinical examination, was hemodynamically stable, BP 100/60 mm Hg, HR 99/min, with Oxygen saturation of arterial blood (Sa O2) of 97%. Biologically, the neutrophilic leukocytosis was detected (12.4 X 10 3/ul with 78.7% PMN), a troponin (TnI) of 0,001 ng/ml (normal range 0.00-0,02 ng/ml), a MB isoenzyme of creatine kinase (CKMB) of 26 U/l (normal range 2-25 U/l), with a subsequent increase to 36 U/l, and a negative urine qualitative toxicology screening.
Figure 1. Resting electrocardiogram on admission. Sinus rhythm, 65/min, QRS axis +90 degrees, biphasic T +/- in DII, DIII, AVF, ST eveletion 2 mm in V1, V2, with negative T in V3-V5.
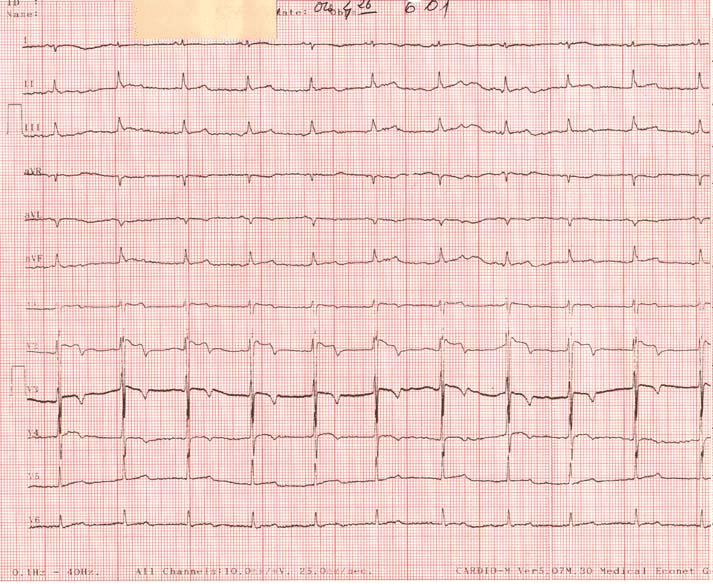
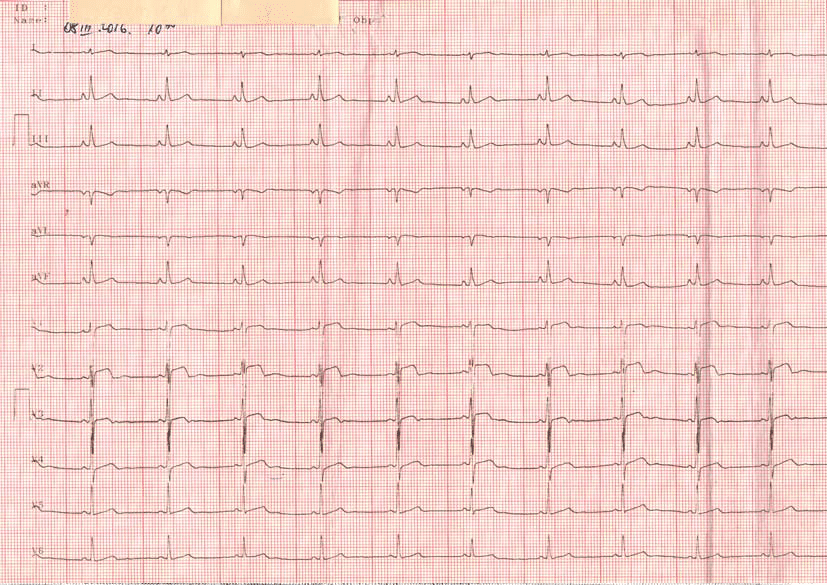
Figure 2. Resting electrocardiogram on admission in Medical Clinic. Sinus rhythm 75/min, QRS axis +90 degrees, increase of ST elevation in V2, V3, T negative in V2-V4, disappearance of changes in the inferior territory
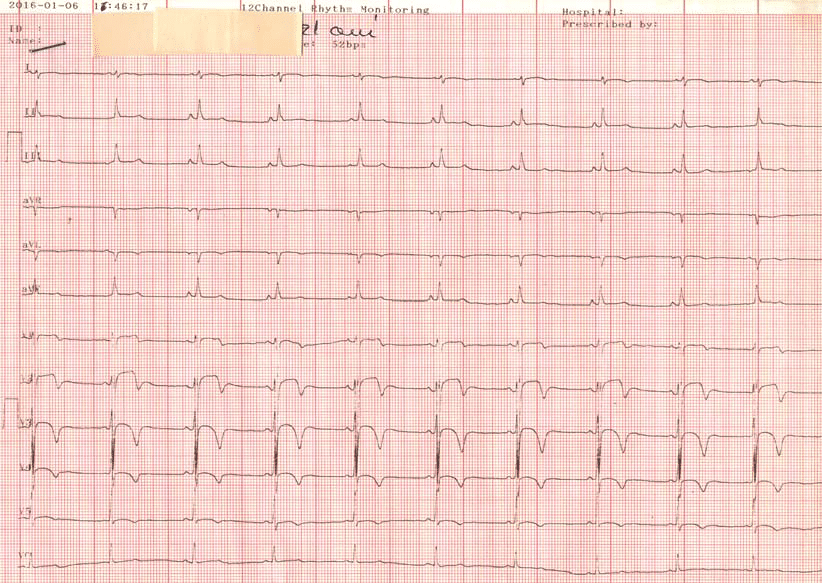
Figure 3. Wandering Pacemaker and the persistency of elevation in V2, V3 and ample T waves, negative in V2-V4.
The next day, CKMB was within normal limits and troponin remained normal. Upon arrival in the clinic, ECG (Figure 2) showed SR 75/min, and increase of ST elevation in V2, V3, with negative T wave in V2-V4, and disappearance of changes in the inferior territory. Two hours later, the ECG shows wandering atrial pacemaker and the persistency of elevation in V2, V3
with ample negative T waves in V2-V4 (Figure 3), pattern maintained during two more days of hospitalization. The emergency transthoracic echocardiography de tec ted hypokinesis of the interventricular septum (IVS) and left ventricle (LV) anterior wall, with rare extra systoles during examination, left ventricular ejection fraction (LVEF) 47%, shortening fraction (SF) 23%,
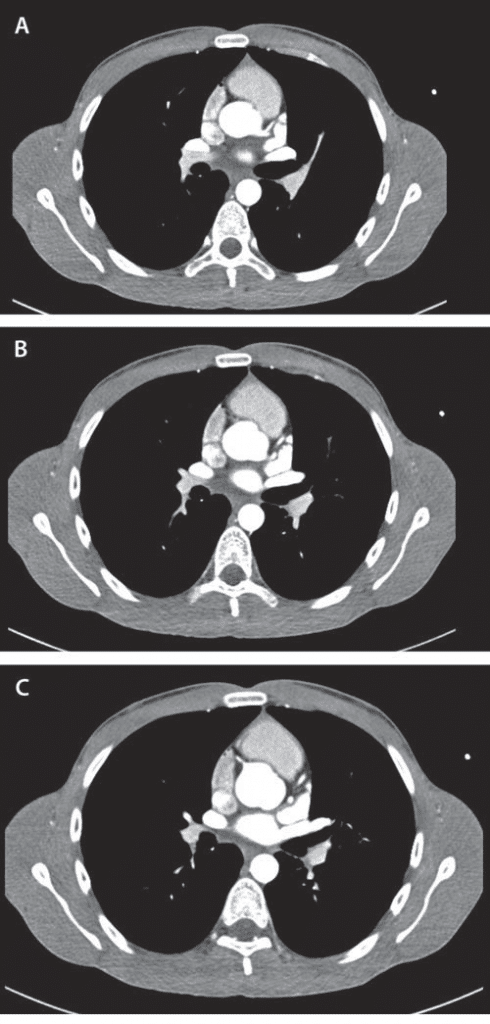
and cardiac cavities normal in size. The CT coronary angiography performed the day after admission revealed a normal appearance of the epicardial coronary arteries (Figure 4A, 4B, 4C).
The evolution was favourable during hospitalization, with gradually normalization of ECG and of the biological tests, as well as the correction of systolic function parameters (EF 51%, SF 27%) and the improvement of the segmental kinetic disorders described, after treatment with oxygen, anticoagulants, dual antiplatelet therapy, statin, beta-blocker and retard nitrate. Although the ethnobotanics products, smoking and alcohol were forbidden, the patient returned one month after the hospital discharge with the same symptoms after smoking a recreational cigarette, with
normal ECG at the time of presentation (Figure 5) and reoccurrence of ischemic changes one hour after admission (Figure 6). During the second hospitalization, he had a simple evolution on therapy.
DISCUSSION
The consumption of ethnobotanics is not frequently associated with the acute coronary syndrome. In literature, only a few cases of acute myocardial infarction (AMI) are cited, associated most commonly with cannabis consumption, and the etiology of this phenomenon is still unknown1. The fi rst case reported in literature was in 1979, a severe case of AMI associated with marijuana consumption, in a patient who had also normal coronary arteries4. The action of cannabinoids is mediated by the stimulation of the sympathetic nervous system through the release of norepinephrine, proved by the fact that it determines the increase of the cardiac debit by more than 30%5. The marijuana can increase the heart rate by 20%-100%, an increase dependent on the
dose consumed, thus increasing the oxygen demand of myocardium1,6.
Figure 4A. CT-Coronary angiography reveals normal LAD at the origin and proximal segments; B. Normal LAD, circumfl ex artery median segments; C. Normal RCA.
There are studies mentioning that marijuana increases the risk of AMI by 4.8 times in the fi rst hour after consumption and that it is responsible for transient ischemia and strokes1,7. There are very little data on pharmacokinetics and pharmacodynamics of synthetic cannabinoids, there were in vitro studies, but data about all symptoms and duration of effects caused by their consumption still remain unknown8. The initial management of these patients should include the ECG tracing of arrhythmias, of myocardial ischemia and screening for various substances potentially consumed. The patient presented is a young adult, with no significant past medical history or family history of premature cardiac disease. It is important to note that the drug testing was negative, including for cocaine, amphetamines and tetrahydrocannabinol (THC). The presence of synthetic cannabinoids (often undetectable in urine drug screening) or other vasoactive substances is very probable. Given the ECG appearance at the time of the presentation (Figure 2), a differential diagnosis with Wellens syndrome is required, but the patient does not have a history of angina and CT- coronary angiography exam doesn’t highlight an occlusion or stenosis of the anterior descending artery, a necessary criterion in defi ning Wellens syndrome. We interpret the ECG changes as an expression of coronary vasospasm, mainly because CT-coronary angiography was normal, the ECG changes were transient and the fact that ethnobotanicals produce the increase of the sympathetic tone, and its involvement in the triggering of the coronary arterial spastic response is well known9.
Figure 5. ECG in ED on second presentation. Normal morphology.
Figure 6. ECG one hour after admission in the Medical Clinic. Sinus rhythm 64/min, intermediate QRS axis, ST elevation in V2, V3.
CONCLUSIONS
Given the fact that the thoracic pain in the young adult is a symptom often found in ED, and AMI in young adult is a pathology quite rare, the physician must take into account the possible consumption of illicit drugs in the differential diagnosis of thoracic pain and myocardial ischemia, and should keep in mind that the synthetic cannabinoids are not seen frequently in the urine drug testing. Such patients, whose history is positive for consumption of ethnobotanics, require monitoring of the ECG and biological tests. Conflict of interest: none declared.
References
1. Arshid Mir, Adebisi Obafemi, Amy Young and Colin Kane.Myocardial Infarction Associated With Use of the Synthetic Cannabinoid K2. Pediatrics 2011;128:1622-1627.
2. Kocabay G, Yildiz M, Duran N, Ozkan M.Acute inferior myocardial infarction due to cannabis smoking ina young man.J Cardiovasc Med (Hagerstown).2009;10(9):669-670
3. Hodcroft CJ, Rossiter MC, Buch AN. Cannabis-associated myocardial infarction in a young man with normal coronary arteries. J Emerg Med.2014 Sep;47(3):277-81
4. Charles R, Holt S, Kirkham N.Myocardial infarction and marijuana. Clin Toxicol.1979;14(4):433-438.
5. Leblanc A1, Tirel-Badets A, Paleiron N, Castellant P, Cornily JC, Andre M, Grassin F, Feuvrier Y, Blanchard C, Zagnoli F, Quiniou G, Vinsonneau U. Cannabis and myocardial infarction without angiographic stenosis in young patient: guilty or not guilty? A case report. Ann Cardiol Angeiol (Paris). 2011 Jun;60(3):154-8.
6. Mittleman MA, Lewis RA, Maclure M, Sherwood JB, Muller JE. Triggering myocardial infarction by marijuana. Circulation 2001;103(23): 2805-2809.
7. Barnes D, Palace J, O’Brien MD. Stroke following marijuana smoking. Stroke. 1992;23(9):1381.
8. Travis S. Heath, Pharm D, Zachary Burroughs, MD, A. Jill Thompson, Pharm D, and Frederick W Tecklenburg, MD. Acute Intoxication Caused by a Synthetic Cannabinoid in Two Adolescents. J Pediatr Pharmacol Ther 2012;17(2):177-181
9. Pozzati A, Pancaldi LG, Di Pasquale G, Pinelli G, Bugiardini P. Transient sympathovagal imbalance triggers “ischemic” sudden death in patients undergoing electrocardiographic Holter monitoring. J Am Coll Cardiol. 1996; 27: 847-852.
 This work is licensed under a
This work is licensed under a